- About
- Mission Statement
Education. Evidence. Regrowth.
- Education.
Prioritize knowledge. Make better choices.
- Evidence.
Sort good studies from the bad.
- Regrowth.
Get bigger hair gains.
Team MembersPhD's, resarchers, & consumer advocates.
- Rob English
Founder, researcher, & consumer advocate
- Research Team
Our team of PhD’s, researchers, & more
Editorial PolicyDiscover how we conduct our research.
ContactHave questions? Contact us.
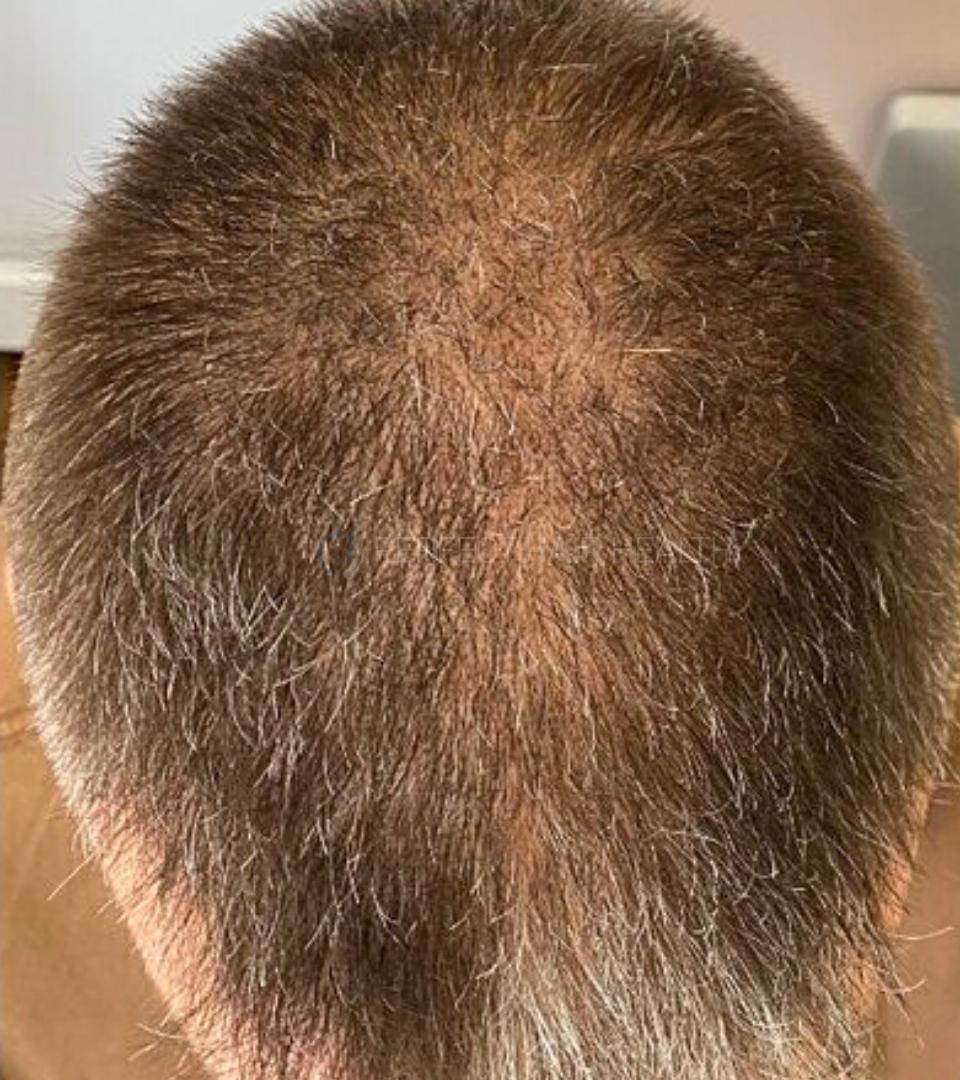
Before-Afters- Transformation Photos
Our library of before-after photos.
- — Jenna, 31, U.S.A.
I have attached my before and afters of my progress since joining this group...
- — Tom, 30, U.K.
I’m convinced I’ve recovered to probably the hairline I had 3 years ago. Super stoked…
- — Rabih, 30’s, U.S.A.
My friends actually told me, “Your hairline improved. Your hair looks thicker...
- — RDB, 35, New York, U.S.A.
I also feel my hair has a different texture to it now…
- — Aayush, 20’s, Boston, MA
Firstly thank you for your work in this field. I am immensely grateful that...
- — Ben M., U.S.A
I just wanted to thank you for all your research, for introducing me to this method...
- — Raul, 50, Spain
To be honest I am having fun with all this and I still don’t know how much...
- — Lisa, 52, U.S.
I see a massive amount of regrowth that is all less than about 8 cm long...
Client Testimonials150+ member experiences.
 Scroll DownPopular Treatments
Scroll DownPopular Treatments- Treatments
Popular treatments. But do they work?
- Finasteride
- Oral
- Topical
- Dutasteride
- Oral
- Topical
- Mesotherapy
- Minoxidil
- Oral
- Topical
- Ketoconazole
- Shampoo
- Topical
- Low-Level Laser Therapy
- Therapy
- Microneedling
- Therapy
- Platelet-Rich Plasma Therapy (PRP)
- Therapy
- Scalp Massages
- Therapy
More
IngredientsTop-selling ingredients, quantified.
- Saw Palmetto
- Redensyl
- Melatonin
- Caffeine
- Biotin
- Rosemary Oil
- Lilac Stem Cells
- Hydrolyzed Wheat Protein
- Sodium Lauryl Sulfate
More
ProductsThe truth about hair loss "best sellers".
- Minoxidil Tablets
Xyon Health
- Finasteride
Strut Health
- Hair Growth Supplements
Happy Head
- REVITA Tablets for Hair Growth Support
DS Laboratories
- FoliGROWTH Ultimate Hair Neutraceutical
Advanced Trichology
- Enhance Hair Density Serum
Fully Vital
- Topical Finasteride and Minoxidil
Xyon Health
- HairOmega Foaming Hair Growth Serum
DrFormulas
- Bio-Cleansing Shampoo
Revivogen MD
more
Key MetricsStandardized rubrics to evaluate all treatments.
- Evidence Quality
Is this treatment well studied?
- Regrowth Potential
How much regrowth can you expect?
- Long-Term Viability
Is this treatment safe & sustainable?
Free Research- Free Resources
Apps, tools, guides, freebies, & more.
- Topical Finasteride Calculator
- Interactive Guide: What Causes Hair Loss?
- Free Guide: Standardized Scalp Massages
- 7-Day Hair Loss Email Course
- Ingredients Database
- Interactive Guide: Hair Loss Disorders
- Treatment Guides
- Product Lab Tests: Purity & Potency
- Evidence Quality Masterclass
More
Articles100+ free articles.
-
Cannabidiol (CBD) Increases Hair Counts By 246%? Not So Fast.
-
Creatine: Does It Worsen Hair Loss? It Depends On The Hair Loss Type.
-
Can Progesterone Improve Hair Regrowth?
-
CRABP2: Can This Gene Predict Regrowth From Retinoids?
-
BTD: Can This Gene Predict Regrowth From Biotin?
-
COL1A1: Can This Gene Predict Regrowth From Collagen Support?
-
2dDR For Hair Loss: What Do We Know So Far About This Sugar?
-
CYP19A1: Can This Gene Predict Regrowth From Hormone Therapy?
PublicationsOur team’s peer-reviewed studies.
- Microneedling and Its Use in Hair Loss Disorders: A Systematic Review
- Use of Botulinum Toxin for Androgenic Alopecia: A Systematic Review
- Conflicting Reports Regarding the Histopathological Features of Androgenic Alopecia
- Self-Assessments of Standardized Scalp Massages for Androgenic Alopecia: Survey Results
- A Hypothetical Pathogenesis Model For Androgenic Alopecia:Clarifying The Dihydrotestosterone Paradox And Rate-Limiting Recovery Factors
Menu- AboutAbout
- Mission Statement
Education. Evidence. Regrowth.
- Team Members
PhD's, resarchers, & consumer advocates.
- Editorial Policy
Discover how we conduct our research.
- Contact
Have questions? Contact us.
- Before-Afters
ArticlesAlopecia Areata: Causes, Treatments, & Why It’s Reversible | 2020 Review
First Published Jul 14 2020Last Updated Oct 29 2024Pharmaceutical Researched & Written By:Perfect Hair Health Team
Researched & Written By:Perfect Hair Health Team Reviewed By:Rob English, Medical Editor
Reviewed By:Rob English, Medical Editor
Want help with your hair regrowth journey?
Get personalized support, product recommendations, video calls, and more from our researchers, trichologists, and PhD's dedicated to getting you the best possible outcomes.
Learn MoreArticle Summary
Alopecia areata (AA) is an autoimmune form of hair loss that impacts 2% of people worldwide. It’s caused by an unknown driver of inflammation that disrupts hair follicle stem cells, leading to slick-bald patches and (sometimes) exclamation-mark hairs. Fascinatingly, AA can spontaneously reverse in 34-50% of patients. Even in cases of long-standing AA, fecal microbiota transplants have led to incredibly hair recoveries. Read on to learn the science behind AA: what we know, what we don’t, and the treatment breakthroughs that may make this hair loss disorder a thing of the past.
Full Article
Alopecia areata is an autoimmune form of hair loss that affects 2% of people worldwide. If you’re dealing with alopecia areata, the burden of hair loss often feels overwhelming – as the condition can progress rapidly, inexplicably, and without regard.
Fortunately, alopecia areata is treatable. In many cases, it’s also reversible. The first step toward making progress? Understanding alopecia areata, its myriad triggers, and how these factors relate to your unique hair loss situation.
In this article, we’ll uncover the characteristics of alopecia areata: its clinical presentations, histological features, and more. We’ll also dive into alopecia areata’s causes: what we know, what we don’t, and what this type of hair loss can tell us about our health.
Finally, we’ll outline treatments for alopecia areata (both conventional and natural): the research supporting them, the expectations for regrowth, and who might be the best candidates for each intervention.
What is alopecia areata?
Alopecia areata (AA) is a form of hair loss driven by autoimmunity. To put it simply, alopecia areata occurs when our bodies mistakenly recognize our hair follicles as foreign invaders, and then begin to attack our hair follicles. This leads to the dysfunction of hair follicle stem cells, and eventually, hair loss.
What does alopecia areata look like?
You might know alopecia areata (AA) from its “patchy” presentation, whereby slick-bald patches begin to form in a non-uniform fashion. But AA can also vary in appearance – and even mask the look of many other common hair loss disorders.
Types of alopecia areata
Alopecia areata focalis or “patchy” alopecia areata Hair loss in patches, can extend beyond just the scalp. The most common form of alopecia areata. It may or may not progress into alopecia totalis or alopecia universalis. 
Alopecia areata totalis Loss of all hair on the scalp including eyelashes and eyebrows. 
Alopecia areata universalis Hair loss of the scalp, eyelashes, eyebrows, and whole body, including all body hair. 
Ophiasis or alopecia areata marginata Hair loss around the circumference of the head in a band-like fashion. It is most commonly seen behind the ears and the nape of the neck, but can occur in the frontal hairline and extend throughout the scalp in severe cases, as well. 
Ophiasis inversus Hair loss that begins in the center of the scalp and progresses into the surrounding regions. 
Alopecia areata incognita Diffuse hair loss whereby no specific bald “patches”, normally characteristic of alopecia areata, can be distinguished. 
What’s the histology of alopecia areata?
Histology is a term used to describe a close-up view of a tissue’s structure. In the world of hair loss, histology refers to the microscopic view of a hair follicle (i.e., what a hair follicle looks like when biopsied).
When doctors are uncertain about someone’s hair loss diagnosis, they’ll often take a biopsy of their patient’s scalp so that they can get a look of the histological features of the affected hair follicles. Then, they’ll compare what they see against the histological hallmarks of certain hair loss disorders.
It might sound invasive, but these scalp biopsies are perhaps the most effective way for dermatologists to definitively diagnose someone’s hair loss. And when it comes to alopecia areata, this type of hair loss has a lot of interesting features:
- Inflammation. Specifically, the infiltration of lymphocytes near hair follicle stem cell bulges. Lymphocytes are immune cells; the bodies uses them as part of an inflammatory response. Where there are high lymphocytes, there are usually high amounts of inflammation. One study found that 84% of alopecia areata subjects presented with this kind of inflammation.
- Dysfunctional hair follicle stem cell bulges. Hair follicle stem cells contain the blueprints to make new hair follicles. When too many lymphocytes collect near these stem cells, they generate inflammation, and that inflammation interferes with the ability for these stem cells to function. This leads to stem cell dysfunction and an inability to form new hair.
- Hair follicle miniaturization. This is a decrease in hair strand diameter, which leads to thinner-looking hair. One study observed that 90% of alopecia areata subjects had hair follicle miniaturization. Conversely, this study only found miniaturization in 25% of subjects. This study found that the presence of miniaturization is likely dependent on the nature of the hair loss – for example, early stages of AA likely do not present with miniaturization. It is most commonly often found in recurrent and chronic forms of AA.
- Increased number of catagen hairs. This study found that 93% of patients presented with an abnormally high number of hair follicles in the catagen phase – the phase in the hair cycle whereby nutrient supply is cut off and the hair prepares to shed. In healthy scalps, only 1% of hair follicles are typically in catagen. With AA, that percent can skyrocket.
Isn’t inflammation & hair follicle miniaturization part of androgenic alopecia (AGA)?
Yes.
Pattern hair loss, also known as androgenic alopecia (AGA), is also often defined by the presence of inflammation, hair follicle miniaturization, and even an increased number of catagen and telogen hairs. This begs the question: how can we distinguish between AGA and alopecia areata… especially in cases where alopecia areata is diffuse?
Well, there are some additional factors that can help us identify if we’re dealing with alopecia areata (AA) or androgenic alopecia (AGA).
What makes alopecia areata (AA) unique from androgenic alopecia (AGA)?
- The patterning of AA. In most AA cases, hair loss begins in a “patchy” fashion — a patterning that is exclusive to AA. In contrast, AGA occurs in a very different, yet still distinct manner. For men, it’s temple recession and crown thinning. For women, it’s most often a widening of the part while their hairline stays intact (also known as a “Christmas tree” pattern).
- Exclamation-point hairs in AA. Exclamation point hairs, pictured below, are a phenomenon only observed in AA. These hairs remain thick along the shaft but are noticeably thinner towards the opening of the follicle, creating an appearance akin to that of an exclamation mark ( ! ). This is only a defining factor if hair is still present.
-
Exclamation mark (!) hair

-
- Pigment casts in AA. Melanin is a substance produced by cells to create pigment for our skin and hair. Interestingly, in cases of AA, there are often “clumps” of melanin deposits throughout the follicular unit. This can appear like a small, dark tattoo where there should be a hair follicle. The incidence of pigment casts varies from study to study from 44% to 72%. Having said that, pigment casts by themselves aren’t a good indicator of AA – mostly because they’re often observed at similar rates in other hair loss disorders like trichotillomania (i.e., a “hair-pulling disorder”).
What causes alopecia areata?
To reiterate from earlier, inflammation seems to initiate of AA. The process looks like this:
- Inflammatory cells infiltrate the area surrounding a hair follicle stem cell bulge.
- This inflammation disrupts stem cell functionality, leading to stem cell dysfunction.
- These dysfunctional stem cells stop producing normal-looking hair follicles.
This leads to:
- Rapid hair follicle miniaturization (i.e., exclamation hairs).
- A loss of visible hair (i.e., slick-bald patches in alopecia areata focalis).
- Weaker, brittler hair that breaks off soon after growing out of the skin surface.
This begs the question… when it comes alopecia areata, what causes the inflammation that kickstarts the whole process?
What causes the inflammation in alopecia areata?
While the exact origin of inflammation isn’t known, researchers have a good idea of three contributing factors: genetics, environmental triggers, and loss of immune privilege in the follicle.
And though we don’t know the exact nature of these contributing factors, researchers have begun to uncover some of the details:
- Genetics. Studies have shown that AA is common among family members, affirming the role of a genetic component in certain cases. Specific genes affected include those that code for immune cell receptors, cell death coordination, immune-regulating cells, other proteins that regulate cellular communication.
- Environmental factors. Much like genetics, environmental elements faced by AA-affected families might also explain why this condition tends to appear multiple times within the same family. These environmental factors include
- Stress
- Infections
- Hormone fluctuations
- Dysbiosis of the gut flora
- Oxidative stress
- Soy consumption (implicated in animal studies, though not yet confirmed in human studies)
- Nutrient deficiencies (specifically, vitamin A and/or vitamin D deficiency.
- Loss of immune privilege. Under normal circumstances, a hair follicle produces its own “shield” from our own immune system. This shield is comprised of many immune-suppressing molecules. This is known as immune privilege, and it’s what make hair follicles incredibly unique mini-organs. However, in AA, researchers believe this immune privilege collapses – preventing the hair follicle from protecting itself against a damaging attack by the immune system. This would lead to inflammation and, thereby, the destruction of the hair follicle stem cell bulge. How this occurs is unknown, but researchers believe it is a result of proteins secreted by skin cells that the body forms an “antibody” to, leading to an immune attack.
What are the available treatments?
Currently, there are a variety of drug and non-drug treatments for AA. But before we reveal them, there are two things worth mentioning:
- Because we don’t fully understand why AA occurs, the most well-studied treatments primarily focus on suppressing the signals that lead to AA (as opposed to treating its root cause). More recent research has explored treatments that try to target some of these potential root causes. These studies show promise, but they’re also a little “out there” in terms of peoples’ comfortabilities. So, as you read on, keep this in mind.
- When it comes to reversing alopecia areata, 34-50% of cases resolve spontaneously. This makes it hard to know which treatments work, and which treatments just happened to coincide with spontaneous reversals. This is why control groups are so important in AA studies. Moreover, the likelihood of spontaneous reversal depends highly on the progression of the disease: as AA progresses, the likelihood of spontaneous resolution declines.
Regardless of these factors, it seems like treating AA in earlier stages leads to better outcomes and decreases the risk of future treatment resistance. So, if you’re facing AA right now, it’s best not to place your bets on a spontaneous reversal; rather, hedge those bets with the treatment options at your disposal (or at least the ones you’re comfortable trying).
The following sections detail many conventional and alternative treatments: the evidence, best practices, mechanisms of action, and more.
Drug-based treatments
Topical, intralesional, and systemic steroids (first line of treatment)
- Best candidates: Patchy AA may be controlled with topical or intralesional steroids. More severe or resistant cases (alopecia totalis, alopecia universalis, ophiasis) may require systemic steroid treatment or combination therapy (steroids + other treatments).
- Mechanisms of action: Reduction of inflammation.
- Dosages: For topical steroids, concentrations vary from 0.05% to 0.25%; for intralesional steroids, most commonly-used agent is triamcinolone acetonide, at concentrations of 2.5 mg/mL to 10 mg/mL; for systemic steroids, varying doses given as pulse doses, a.k.a large bolus doses for a specific period of time, administered in intervals.
- Outcomes: Results vary between methods of administration. Topical steroids are best suited to earlier stages of AA, with about 57% of these patients demonstrating complete regrowth. Intralesional steroids have a slight advantage over topicals, with 63% of patients achieving complete growth in one study. Systemic steroid treatment is primarily relegated to resistant cases.
- Problems: With topical and intralesional treatment, the main side effect is cutaneous atrophy or thinning of the skin. Systemic steroids come with a higher risk of side effects, and these risks may outweigh the benefits of hair growth. The relapse rate after steroid treatment ranges between 33% and 75%.
Janus kinase (JAK) inhibitors (oral and topical)
- Best candidates: Men, women, and children with patchy AA, alopecia universalis, alopecia totalis, according to preliminary evidence.
- Mechanisms of action: Blocks inflammatory signaling.
- Dosages: 5mg twice per day.
- Outcomes: Efficacy is similar in patchy alopecia areata, alopecia universalis, and alopecia totalis as well as in both men vs. women and adults vs. children. Oral administration is more likely to produce a good response when compared to the use of topical applications. Studies show initial hair growth occurs as soon as 2 months, with full regrowth occurring in an average of 6 months.
- Problems: Evidence is limited and primarily in the form of case reports. As such, though JAK inhibitors show promise, we don’t know a lot about the safety or efficacy of these medications in AA, yet. Drugs in this class have been linked to an increased risk of upper respiratory issues, latent virus reactivation, and cancer. The exact risk of these adverse effects in the treatment of AA is unknown, however, upper respiratory infection was the most common among available case studies. Like other therapies in AA, there is a high rate of relapse after cessation of the drug.
Immunotherapy (dinitrochlorobenzene, squaric acid dibutylester and diphenylcyclopropenone, with diphenylcyclopropenone)
- Best candidates: Mild to moderate patchy alopecia areata.
- Mechanisms of action: Immunogenic compound “distracts” the immune system with a more stimulating antigen than the self-antigen the mediates the autoimmune reaction.
- Dosages: Concentration sufficient enough to induce an allergic response.
- Outcomes: Response rates as reported in the literature range widely, from about 9% to 87%. About 20% to 30% of patients are able to achieve significant hair growth, such that they are able to manage their hair loss without a wig. This specific therapy may require longer treatment times, as evidenced by over a two-fold increase in response rate at 32 months versus 6 months. So, ask your doctor about whether a longer treatment period might be right for you. In over 30 years of use, long-term side effects have not been reported with immunotherapy, however, some side effects can occur during therapy. The most common side effect is cervical and occipital lymphadenopathy and severe dermatitis, however, these only last for the duration of the therapy. Moreover, dermatitis can be avoided by using the proper concentration of the antigenic compounds. Vitiligo and itching have also been reported but are considered rare. Overall, the treatment appears to be well-tolerated and effective.
- Problems: As with most treatments, relapse rates are high at around 62%. Response rates are somewhat low when administered for the same treatment periods as other treatments. In other words, immunotherapy takes longer to work than other treatments.
Minoxidil
- Best candidates: Mild patchy AA, AA patients tapering off of steroid therapy
- Mechanisms of action: Not fully known, but is believed to stimulate the “anagen” growth phase of the hair cycle, thereby promoting regrowth of lost hairs.
- Dosages: 2% or 5% minoxidil, two to three times daily.
- Outcomes: In one study, 85% of patients using 5% minoxidil alone experienced regrowth, however, this regrowth wasn’t cosmetically significant. Another study demonstrated that the application of 2% minoxidil, when applied three times daily, helped retain hair regrowth after tapering off of steroid treatment.
- Problems: Minoxidil doesn’t seem to be that effective outside of post-steroid hair retention.
Methotrexate
- Best candidates: Moderate to severe AA, including universalis, diffuse, and totalis phenotypes.
- Mechanisms of action: Suppression of the immune system.
- Dosage: 10-25mg per week + folate/folic acid supplements (methotrexate depletes folic acid).
- Outcomes: One study reported that 44.4% of subjects taking methotrexate were able to regain 50% or more of their hair as observed in a follow-up period ranging from 3 to 51 months. The best responders were males, those with multifocal patchy AA (followed by totalis, then universalis, and, lastly, diffuse), and those who used a cumulative dose of 1,000 to 1,500mg. When corticosteroids were used alongside methotrexate, the number of patients regrowing at least 50% of their hair increased to 77.3%.
- Problems: Methotrexate isn’t well-studied for AA — the evidence is primarily made up of case studies. 3-24% of patients can expect to experience side effects like mild to moderate leukopenia, thrombocytopenia, and megaloblastic anemia. There is also the risk of liver fibrosis, with an incidence ranging from 7% to 71.8%. Such a wide range makes the true risk hard to quantify. Myelosuppression is also a dangerous side effect and its risk associated with methotrexate use is unpredictable. Relapse rates vary from 33% to 80%, with some studies suggesting the rate is associated with how much hair is gained during treatment — more hair regrowth during treatment is associated with a lower risk of relapse after treatment.
Non-drug based treatments
Fecal microbiota transplant (FMT)
Fecal microbiota transplant (FMT) is a procedure whereby gut bacteria are isolated from a donor’s feces, purified, and then transplanted into an FMT candidate. This is the only procedure in which bacterial strains that have been lost from the gut can be reinoculated.
Currently, the procedure is elective in Europe (anyone can elect to have it performed). But in the U.S., it’s only available for chronic C. difficile infections. In the U.K., Taymount Clinic is one of the most popular worldwide-serving clinics for elective FMT.
- Best candidates: Evidence is limited but FMT has been used to treat patchy AA and alopecia universalis. May also be effective in treatment-resistant cases.
- Mechanisms of action: Unknown, but probably a normalization of the gut flora, leading to reduced autoimmune activity.
- Dosage: N/A; donor transplant is performed in one procedure, although people often elect for multiple procedures (depending on the delivery method).
- Outcomes: There are currently three case studies (studies here and here) investigating the efficacy of FMT in AA: two in alopecia universalis and one in patchy AA. Of the 3 case studies, all patients showed marked improvement following FMT — with two cases of almost full regrowth (one in universalis alopecia and one in patchy AA) and one case of partial regrowth. In all cases, this hair regrowth was sustained for at least 1.5 to 3 years. Considering the relapse of AA for most treatments is high, this sustained regrowth is promising. However, whether or not this regrowth was sustained beyond the follow-up period is unknown.
- Problems: FMT is still considered an investigative treatment in the U.S. and is, therefore, not elective for individuals with AA, unless a patient is also dealing with chronic C. difficile infection. As such, US residents wanting to explore the treatment must travel for the procedure and pay for it out-of-pocket — these costs can rack up (but may be worth it in the long run).
FMT before & after photos
Case #1: (A) 1 month, (B) 4 months, (C) 1.5 years after FMT in patchy AA
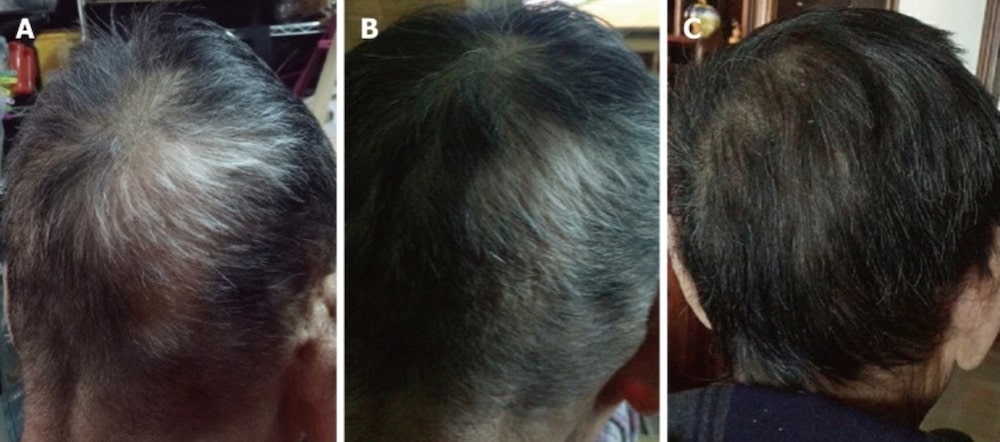
Case #2: (A) The patient’s scalp when his AA first began (B) a few months, (C) 1.5 years after FMT in alopecia universalis

Case #3: The beginning of hair regrowth after FMT in a case of long-standing alopecia universalis
Essential oils
- Best candidates: Evidence is limited, however, efficacy has been demonstrated for general AA in one study. In this specific study, the authors did not specify which kind of AA patients were dealing with.
- Mechanisms of action: Unknown, but probably a reduction in inflammation.
- Dosage: 2 drops thyme essential oil (EO), 3 drops lavender EO, 3 drops rosemary EO, 2 drops cedarwood EO diluted in 3mL jojoba oil and 20mL grapeseed oil.
- Outcomes: In this study, 54% of AA patients in the active group experienced hair regrowth over 7 months while 46% experienced no change (however, hair loss also did not get worse). A majority of these patients achieved hair regrowth in the 10-30% range, followed by 81-100%. In contrast, 78% of the placebo group did not improve, suggesting the essential oil mixture did, indeed, have an effect. It’s likely that the remaining 22% were experiencing spontaneous remission. Neither group experienced adverse side effects.
- Problems: It’s not clear just how many patients may benefit from EO application given that spontaneous resolution is a common occurrence. We see evidence of this in the placebo group, which may be a confounding factor in the measurement of treatment efficacy (since we don’t know how many in the active group would have resolved without intervention). Taking this into account, the response rate, when compared to other treatments for AA, is relatively low. Another issue is the fact that the study did not have a designated follow-up period to measure the rate of relapse. Therefore, we can’t be sure of just how effective this treatment is in the long run. Moreover, the treatment period was quite long in comparison to what is normally employed with other therapies. Given that AA can become more treatment-resistant as time goes on, using topical EOs may delay appropriate treatment and, as a result, require more aggressive therapies in the future.
Onion juice
- Best candidates: Men and women with patchy AA.
- Mechanisms of action: Unknown, but researchers believe it could work similarly to immunotherapy.
- Dosage: Application sufficient to cover the affected area(s) twice daily.
- Outcomes: This study found that patients with patchy AA were able to see hair regrowth as early as 2 weeks into the study period. Full hair regrowth was seen in 86.9% of patients after 8 weeks. Contrastingly, hair regrowth was only observed in 13% of the control group, making the findings of this study statistically significant.
- Problems: This study, unfortunately, had no follow-up period. As such, we don’t know how many patients experienced a relapse after cessation of treatment. Moreover, the smell of onion juice may make this treatment hard to adhere to long-term.
Garlic gel
- Best candidates: Men and women with mild patchy AA.
- Mechanisms of action: Unknown, but researchers believe it could work similarly to immunotherapy.
- Dosage: 5% garlic gel with 0.1% betamethasone valerate gel, twice daily.
- Outcomes: This study found that garlic was able to enhance the hair growth-promoting effects of a corticosteroid, betamethasone valerate. After 3 months, the active group was able to achieve a significant reduction of hair loss patches — more so than the corticosteroid topical alone.
- Problems: Like the onion juice study, this study (1) did not measure the rate of relapse after cessation of therapy and (2) fails to account for the smell, which may make the treatment difficult to adhere to in real-world settings.
Capsaicin
- Best candidates: Patients with patchy AA and, possibly, alopecia totalis.
- Mechanisms of action: Unknown, but researchers suspect neuroimmunological modulation in the hair follicle.
- Dosage: 0.075% capsaicin topical applied daily.
- Outcomes: Studies employing the use of capsaicin have show varying results. Some studies report the regrowth of vellus hairs, but no appreciable regrowth sufficient to justify its use over other treatments, while others report hair growth in just 3 weeks.
- Problems: Evidence suggests capsaicin may promote some degree of regrowth, but not enough to justify its use over other treatments — especially considering that AA becomes increasingly treatment-resistant over time. Thus, capsaicin use may delay appropriate treatment and, thus, increase the risk of refractory AA in the long-run.
Vitamin D repletion
- Best candidates: Patients with patchy AA and vitamin D deficiency and/or genetically reduced vitamin D receptor expression.
- Mechanisms of action: Likely a modulation of autoimmune activity in the follicle, due to vitamin D’s widespread effects on balancing the immune system.
- Dosage: For oral vitamin D use, the dosage will vary depending on the severity of vitamin D deficiency and whether your practitioner decides to opt for weekly bolus or daily doses. For topical vitamin D therapy, topical applications range from 0.005% calcipotriol twice daily to 50 micrograms/mL calcipotriol once daily.
- Outcomes: Evidence from meta-analyses show that AA patients are more likely to be vitamin D deficient than healthy controls. This would suggest that vitamin D could be beneficial to AA patients, however, no studies have been conducted to assess clinical benefit. The topical application of vitamin D-like, conversely, has been investigated as a treatment avenue. These studies show that twice daily application of various concentrations results that vary from 50% regrowth all the way to clinical remission (full hair regrowth). One study found that efficacy was associated with lower vitamin D levels at the beginning of the study, suggesting that lower vitamin D levels may be a marker of a good candidate. Additionally, one case report demonstrated full clinical remission in a patient with AA and reduced vitamin D receptor expression. Thus, AA patients with low vitamin D levels or reduced vitamin D receptor expression may have the best response to treatment. Studies also show minimal risk of adverse side effects.
- Problems: Studies do not currently show benefit in more severe cases of AA, like alopecia totalis or alopecia universalis. There is limited evidence investigating the therapeutic potential of oral supplements.
Zinc
- Best candidates: Patients with mild AA and zinc deficiency.
- Mechanisms of action: Unknown, but could be attributed to antioxidant regulation and anti-inflammatory activity.
- Dosage: Dosage depends on the severity of the deficiency, however, doses between 50 and 220mg have been used in the literature.
- Outcomes: Studies suggest AA patients have lower zinc levels compared to healthy controls. Interestingly, evidence also suggests a correlation between zinc levels and treatment resistance, meaning zinc deficiency may have an emerging role in refractory AA. However, some studies have failed to find a relationship between zinc and AA. Moreover, some studies show no benefit with zinc supplementation while others suggest zinc therapy may be beneficial in the context of mild AA with zinc levels below 70 μg/dL. Overall, the role of zinc therapy in AA is unclear other than zinc deficiency is more common among AA patients. Nonetheless, zinc repletion may confer health benefits in the presence of deficiency, even if clinical regrowth is not achieved.
- Problems: Research is mixed, with some studies suggesting benefit and others suggest a net zero effect. Thus, there is no conclusive evidence to support the use of zinc in AA.
Azelaic acid
- Best candidates: Patients with patchy AA.
- Mechanisms of action: Unknown, but preliminary evidence suggests it may act similarly to that of immunotherapy.
- Dosage: 20% azelaic acid topical applied twice daily.
- Outcomes: Evidence supporting the use of azelaic acid in patients with AA is lacking. However, one pilot study demonstrates efficacy on par with anthralin, a medication used to treat psoriasis (another autoimmune disease that affects the skin). Just over half of the patients tested achieved complete regrowth with both treatments with no report of adverse events.
- Problems: Research is limited and, as such, the true efficacy of azelaic acid is not known. Moreover, the aforementioned study did not employ a follow-up period, which is necessary to estimate the rate of relapse.
Platelet-rich plasma (PRP)
- Best candidates: Patients with ophiasis-pattern AA resistant to steroid treatment or AA patients who develop side effects with steroid treatment.
- Mechanisms of action: Unknown, possibly immunomodulatory effects.
- Dosage: 9 mL injection.
- Outcomes: In one case study of steroid-resistant ophiasis AA, a form of AA which is generally hard to treat, the patient was able to achieve regrowth by month 1 with significant regrowth by month 3. The patient reported no side effects. Another study demonstrated the superiority of PRP over steroid injections for patchy AA.
- Problems: Unfortunately, there is limited evidence available. The rate of relapse is unknown. The procedure is also costly.
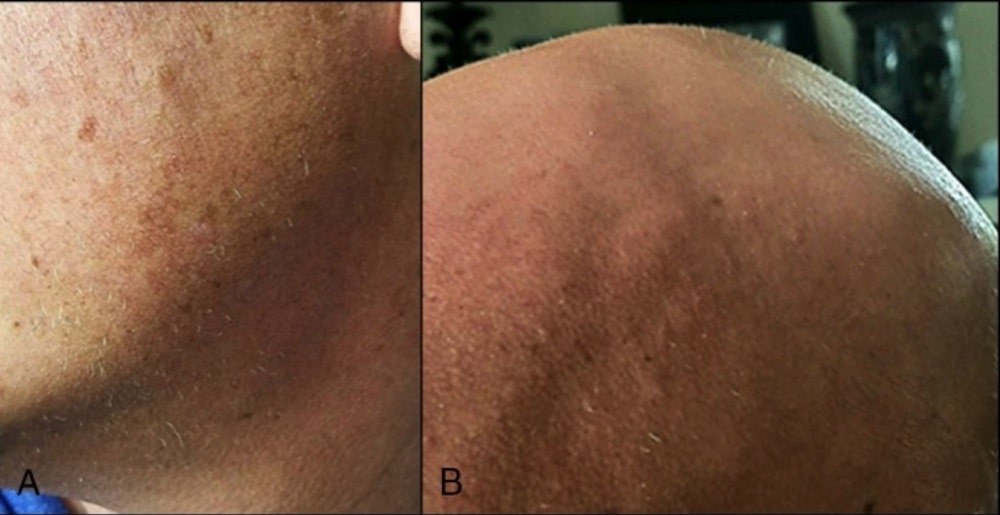
Case study: ophiasis-type AA before and 3 months after PRP treatment.

Brotzu Lotion
Brotzu lotion is a topical formulated by Dr. Brotzu. It contains three main compounds: dihomo-gamma-linoleic acid, S-Equol, and propionyl-L-carnitine — ingredients designed to target inflammation and decreased blood flow in follicles.
There is currently no clinical evidence to support the efficacy of Brotzu lotion in AA. Nonetheless, some initial case studies do show promise. Take, for example, these two before-and-afters:
Brotzu Lotion: a child with alopecia universalis

And here’s a case of near-complete recovery of patchy AA in just 16 months from Dr. Brotzu’s presentation at this conference — start at 10:30):
Brotzu Lotion: alopecia areata recovery
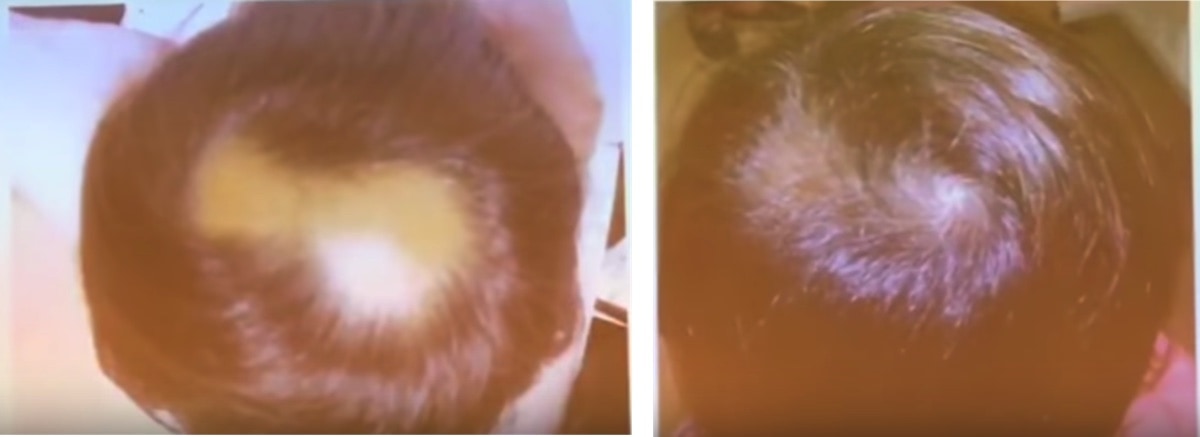
While these are the only case studies we have pictures of, Dr. Brotzu’s patent cites more case studies. This is encouraging for AA patients — especially given it seems confer benefit even in more severe cases, of which are generally more likely to be resistant to treatment.
But it bears repeating: even Dr. Brotzu has claimed it’s difficult to know just how effective the lotion is for AA – mainly because of the spontaneous recoveries.
Helminthic therapy
Helminths, better known as hookworms, are tiny parasites that embed themselves in the small intestines of their hosts.
Helminths are unique in that they have a novel survival mechanism — one that might actually to a broader, modulatory effect on the whole immune system!
The specifics? Helminths “mute” the activity of T-cells, protecting them from destruction by the host’s immune system. This is accomplished through the stimulation of Tregs, a group of cells that reduce the inflammatory potential of the immune system.
As such, in theory, T-cell activity is modulated as a whole, reducing our reactivity to other reactive compounds — including our own tissue. Because auto-reactivity to our own tissue is what mediated autoimmunity (including in AA) reduced T-cell activity may also mean a reduced risk of autoimmunity.
And though research on helminth therapy is still in its infancy, preliminary studies suggest that this evidence might just translate to real-world efficacy. In fact, the therapy has shown promise for a variety of disorders, ranging from inflammatory bowel disorders to allergy all the way to mouse models of multiple sclerosis, an autoimmune disorder.
Considering this evidence, it’s not surprising that Moises Velasquez-Manoff, a male with alopecia totalis, reported hair growth for the first time in years following his experimentation with helminth therapy. He details his experience with helminth self-infection, alongside a historical perspective of helminth eradication, in his book: An Epidemic of Absence.
While this evidence alone is certainly not enough to warrant self-experimentation with helminth self-infection, this emerging research is compelling and underscores the growing importance of the symbiotic relationship of humans and microbes.
Success rates
As seen in the outcomes of the different studies, the likelihood of significant (or complete) recovery is relatively high. And, again, a large proportion of AA patients (34-50%) will spontaneously recover within one year.
This is great news! But, it also makes it difficult to effectively estimate the true success rate of treatments. So, is there any way that someone with AA might be able to gauge their likelihood of recovery (or lack thereof)?
Yes. In clinical practices, there are criteria for AA known as “poor prognostic factors” – i.e., things that might make you less likely to experience full hair recovery. According to the literature, these include:
- Bald patches that persist for longer than 1 year.
- Onset of hair loss before puberty.
- A family history of AA.
- Ophiasis pattern of AA.
- Associated nail changes, a.k.a when nail changes occur alongside AA.
- Atopy, a.k.a a propensity to developing allergic diseases like eczema, asthma, and allergic rhinitis.
So, if you fit into these categories, chances are your AA might be more treatment-resistant. That being said, it doesn’t mean you can’t recover your hair; it just means that you may need to explore more treatment avenues (or combination therapies) to find what works for your hair loss specifically. Your practitioner can help guide you through identifying these treatment avenues.
With that, you’ll also want to consult your doctor early into the process – as treatment resistance can increase as the condition progresses. As such, it’s better to forego experimental / home remedies and begin a treatment plan right away.
This isn’t to say natural therapies might not be an option for you, but, rather that you should discuss the evidence of those treatments with your doctor and, if suited to you, explore the therapy under their supervision.
This will help avoid treatment resistance that may result from delayed treatment, which would partly mitigate a major poor prognostic factor that is within your control.
Summary
Alopecia areata (AA) is a form of autoimmune hair loss characterized by inflammation, exclamation mark hairs, patchy hair loss (in early stages), and hair follicle miniaturization (in later stages). The condition can progress to alopecia totalis (loss of eyebrow and eyelash hairs) or alopecia universalis (loss of hair all over the body). But in many cases, it spontaneously reverses.
An autoimmune attack near the hair follicle stem cell bulge is what triggers AA-related hair loss. This results in inflammation, stem cell dysfunction, a malformed hair follicle, and thereby thiner, brittler hair that is prone to breakage. Eventually, hair cycling also becomes dysfunctional, leading to continued hair growth dysfunction and premature hair fall.
Thankfully, a large proportion of AA cases will spontaneously resolve within a year of onset. Having said that, it’s not a guarantee. So, while “waiting it out” may mean you need no treatment at all, it also poses a risk of progression. The further AA progresses, the higher the likelihood of treatment resistance.
So, it’s important that talk to your doctor when you first notice the hair loss. The earlier you catch it, the better your chances of regrowth. This is especially true if:
- Your hair loss began before puberty
- You have a family history of AA.
- Your hair loss is in the “ophiasis” pattern.
- Your hair loss is associated with nail changes.
- You have concurrent atopy (eczema, asthma, allergic rhintis).
Nevertheless, a wide array of treatment options do exist — both drug-based and non-drug-based – for manageable and refractory cases alike. Generally, corticosteroids are one of the first-line treatments. When corticosteroids aren’t effective, immunotherapy, methotrexate, JAK inhibitors, and alternative treatments (aromatherapy, vitamins/minerals, microbial modulation, and more) are usually explored.
Overall, the prognosis for most AA patients is good. Having said that, the risk of relapse is still high. This is mainly attributed to the fact that most treatments are confined to suppressing the signaling that leads to AA hair loss, as opposed to mitigating the root cause of AA. We just don’t know enough about the origin of AA to target these causes (yet).
The one exception to this rule might be fecal microbiota transplants (FMT) — a treatment that has shown major hair recoveries for long-standing AA patients (who typically don’t respond well to treatment), and no signs of relapse for those responders (at least within study windows of 1.5 to 3 years). However, evidence on FMT is incredibly limited. Moreover, the treatment is currently not readily accessible in the US (unless you have AA and you’re seeking treatment for a chronic C. difficile infection).
Overall, hair regrowth is absolutely possible for most AA patients — whether through natural or conventional means. Just make sure to get in touch with a doctor as soon as you notice your hair loss, so that they can help direct a treatment plan that’s going to be best suited to your condition.
If you have any questions, please feel free to leave them in the comments!
Want help with your hair regrowth journey?
Get personalized support, product recommendations, video calls, and more from our researchers, trichologists, and PhD's dedicated to getting you the best possible outcomes.
Learn More
Perfect Hair Health Team
"... Can’t thank @Rob (PHH) and @sanderson17 enough for allowing me to understand a bit what was going on with me and why all these [things were] happening ... "

 — RDB, 35, New York, U.S.A.
— RDB, 35, New York, U.S.A."... There is a lot improvement that I am seeing and my scalp feel alive nowadays... Thanks everyone. "

 — Aayush, 20’s, Boston, MA
— Aayush, 20’s, Boston, MA"... I can say that my hair volume/thickness is about 30% more than it was when I first started."

 — Douglas, 50’s, Montréal, Canada
— Douglas, 50’s, Montréal, CanadaWant help with your hair regrowth journey?
Get personalized support, product recommendations, video calls, and more from our researchers, trichologists, and PhD's dedicated to getting you the best possible outcomes.
Join Now - Mission Statement