- About
- Mission Statement
Education. Evidence. Regrowth.
- Education.
Prioritize knowledge. Make better choices.
- Evidence.
Sort good studies from the bad.
- Regrowth.
Get bigger hair gains.
Team MembersPhD's, resarchers, & consumer advocates.
- Rob English
Founder, researcher, & consumer advocate
- Research Team
Our team of PhD’s, researchers, & more
Editorial PolicyDiscover how we conduct our research.
ContactHave questions? Contact us.
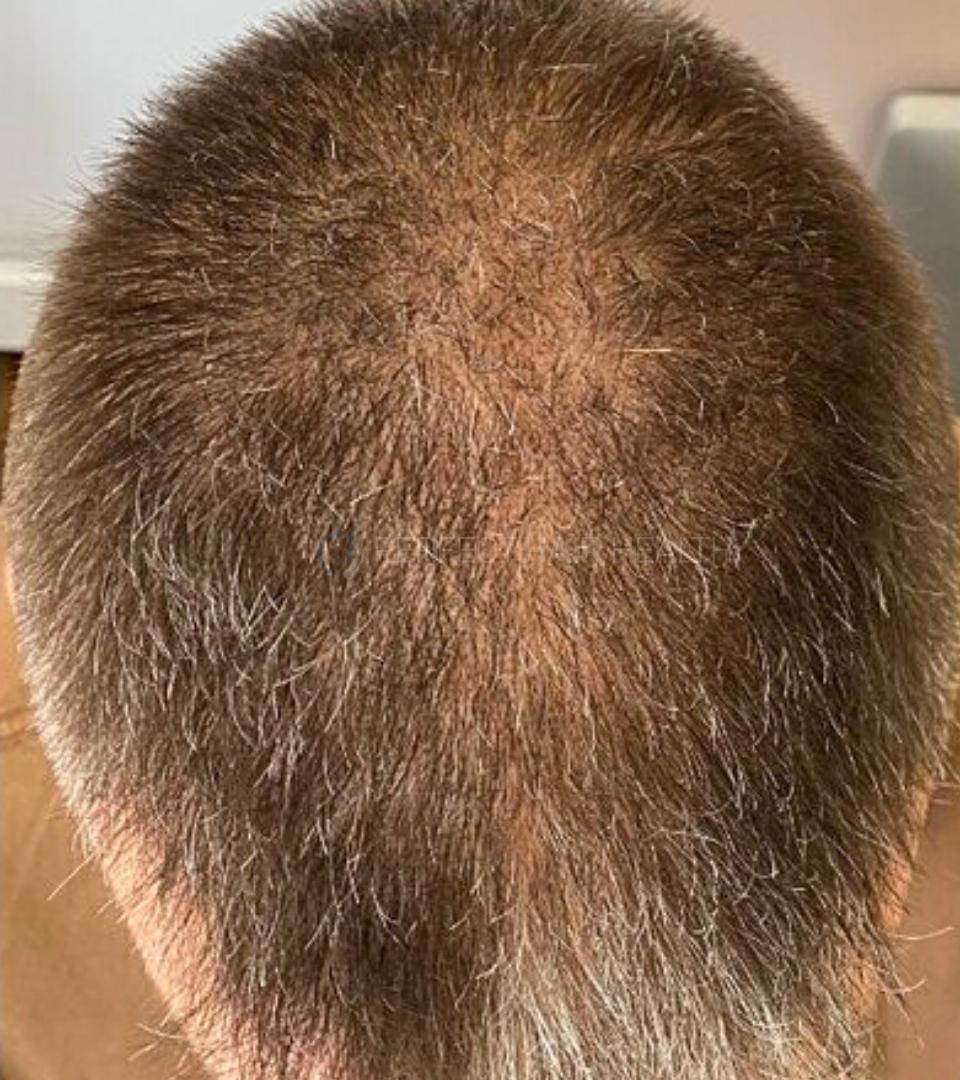
Before-Afters- Transformation Photos
Our library of before-after photos.
- — Jenna, 31, U.S.A.
I have attached my before and afters of my progress since joining this group...
- — Tom, 30, U.K.
I’m convinced I’ve recovered to probably the hairline I had 3 years ago. Super stoked…
- — Rabih, 30’s, U.S.A.
My friends actually told me, “Your hairline improved. Your hair looks thicker...
- — RDB, 35, New York, U.S.A.
I also feel my hair has a different texture to it now…
- — Aayush, 20’s, Boston, MA
Firstly thank you for your work in this field. I am immensely grateful that...
- — Ben M., U.S.A
I just wanted to thank you for all your research, for introducing me to this method...
- — Raul, 50, Spain
To be honest I am having fun with all this and I still don’t know how much...
- — Lisa, 52, U.S.
I see a massive amount of regrowth that is all less than about 8 cm long...
Client Testimonials150+ member experiences.
 Scroll DownPopular Treatments
Scroll DownPopular Treatments- Treatments
Popular treatments. But do they work?
- Finasteride
- Oral
- Topical
- Dutasteride
- Oral
- Topical
- Mesotherapy
- Minoxidil
- Oral
- Topical
- Ketoconazole
- Shampoo
- Topical
- Low-Level Laser Therapy
- Therapy
- Microneedling
- Therapy
- Platelet-Rich Plasma Therapy (PRP)
- Therapy
- Scalp Massages
- Therapy
More
IngredientsTop-selling ingredients, quantified.
- Saw Palmetto
- Redensyl
- Melatonin
- Caffeine
- Biotin
- Rosemary Oil
- Lilac Stem Cells
- Hydrolyzed Wheat Protein
- Sodium Lauryl Sulfate
More
ProductsThe truth about hair loss "best sellers".
- Minoxidil Tablets
Xyon Health
- Finasteride
Strut Health
- Hair Growth Supplements
Happy Head
- REVITA Tablets for Hair Growth Support
DS Laboratories
- FoliGROWTH Ultimate Hair Neutraceutical
Advanced Trichology
- Enhance Hair Density Serum
Fully Vital
- Topical Finasteride and Minoxidil
Xyon Health
- HairOmega Foaming Hair Growth Serum
DrFormulas
- Bio-Cleansing Shampoo
Revivogen MD
more
Key MetricsStandardized rubrics to evaluate all treatments.
- Evidence Quality
Is this treatment well studied?
- Regrowth Potential
How much regrowth can you expect?
- Long-Term Viability
Is this treatment safe & sustainable?
Free Research- Free Resources
Apps, tools, guides, freebies, & more.
- Topical Finasteride Calculator
- Interactive Guide: What Causes Hair Loss?
- Free Guide: Standardized Scalp Massages
- 7-Day Hair Loss Email Course
- Ingredients Database
- Interactive Guide: Hair Loss Disorders
- Treatment Guides
- Product Lab Tests: Purity & Potency
- Evidence Quality Masterclass
More
Articles100+ free articles.
-
Cannabidiol (CBD) Increases Hair Counts By 246%? Not So Fast.
-
Creatine: Does It Worsen Hair Loss? It Depends On The Hair Loss Type.
-
Can Progesterone Improve Hair Regrowth?
-
CRABP2: Can This Gene Predict Regrowth From Retinoids?
-
BTD: Can This Gene Predict Regrowth From Biotin?
-
COL1A1: Can This Gene Predict Regrowth From Collagen Support?
-
2dDR For Hair Loss: What Do We Know So Far About This Sugar?
-
CYP19A1: Can This Gene Predict Regrowth From Hormone Therapy?
PublicationsOur team’s peer-reviewed studies.
- Microneedling and Its Use in Hair Loss Disorders: A Systematic Review
- Use of Botulinum Toxin for Androgenic Alopecia: A Systematic Review
- Conflicting Reports Regarding the Histopathological Features of Androgenic Alopecia
- Self-Assessments of Standardized Scalp Massages for Androgenic Alopecia: Survey Results
- A Hypothetical Pathogenesis Model For Androgenic Alopecia:Clarifying The Dihydrotestosterone Paradox And Rate-Limiting Recovery Factors
Menu- AboutAbout
- Mission Statement
Education. Evidence. Regrowth.
- Team Members
PhD's, resarchers, & consumer advocates.
- Editorial Policy
Discover how we conduct our research.
- Contact
Have questions? Contact us.
- Before-Afters
ArticlesIf I Am Planning a Family, Should I Stop Taking Finasteride? (Men & Women)
First Published Feb 7 2023Last Updated Oct 29 2024Pharmaceutical Researched & Written By:Perfect Hair Health Team
Researched & Written By:Perfect Hair Health Team Reviewed By:Rob English, Medical Editor
Reviewed By:Rob English, Medical Editor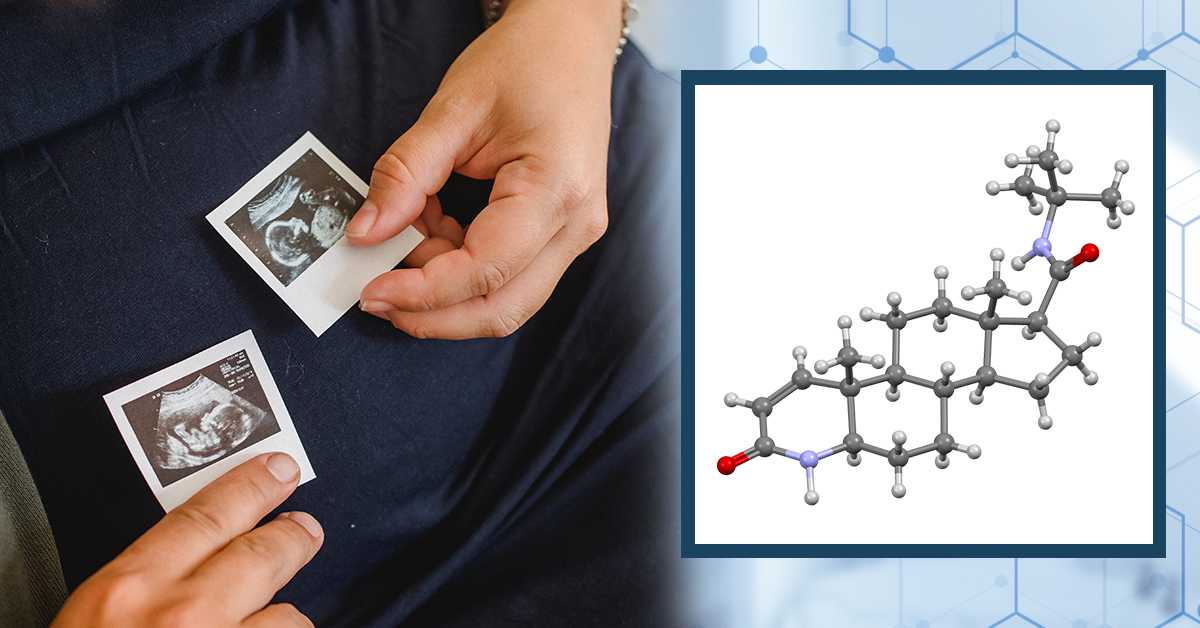
Want help with your hair regrowth journey?
Get personalized support, product recommendations, video calls, and more from our researchers, trichologists, and PhD's dedicated to getting you the best possible outcomes.
Learn MoreArticle Summary
Females using oral finasteride are advised to quit the drug at least one month before conceiving, as well as throughout pregnancy and breastfeeding. But what about men? The evidence is nuanced. Some clinicians claim that finasteride use for men during windows of conception poses no risk to a developing fetus — and that even if with daily unprotected sex during pregnancy, the incidental exposure of finasteride to the fetus (via semen) is 750x lower than what is required to cause damage. On the other hand, case reports indicate that finasteride use may be causally associated with epigenetic changes and DNA fragmentation of sperm — even despite all other markers (i.e., sperm volume, motility, and/or counts) showing no changes. In this article, we’ll dive into the studies, provide our takes on the data, and reveal an alternate strategy for men using finasteride who want to grow their families but also preserve their hair.
Full Article
In the medical literature, it’s well established that women should withdraw from finasteride prior to conceiving, or abstain from finasteride throughout pregnancy and/or while breastfeeding. But what about men? Can they continue using finasteride during conception? What about during their partners’ pregnancy — when indirect finasteride exposure (via semen) might expose the female and fetus to the drug?
The answers and evidence aren’t so straightforward. Fortunately, for those concerned of adverse effects from finasteride on either sperm parameters or developing fetuses, there are strategies to mitigate these risks and continue protecting your hair. This article discusses the data, and elucidates a finasteride dosing strategy for men looking to keep their hair while also growing their family.
Is it Safe for Women to Use Finasteride During Conception?
Probably not. Here’s why.
Drugs like finasteride and dutasteride can bypass the placenta, where they can begin to inhibit 5-alpha reductase activity in a developing fetus and interfere with their hormonal profile.[1]https://rep.bioscientifica.com/configurable/content/journals$002frep$002f155$002f3$002fREP-17-0380.xml The hormone that these drugs reduce — dihydrotestosterone — is less relevant in adulthood, but is critical for early development — particularly for males. Subsequently, animal studies have shown that prolonged finasteride use in pregnant females may mutate and/or inhibit the development of male fetus genitalia.[2]https://dailymed.nlm.nih.gov/dailymed/lookup.cfm?setid=f96c6acd-4d02-4ece-bd54-2d5a35aab7f5#section-12.2
Since it takes ~30 days for finasteride to clear the body, doctors recommend that women trying to conceive should discontinue the drug at least one month before conception. Some doctors even advise their pregnant female patients to avoid any finasteride exposure whatsoever — including any handling of the medication. This is out of an abundance of caution for the safety of the developing fetus.
What About Men? Can Men Use Finasteride During Conception?
When it comes to men using finasteride during windows of conceptions opinions on whether or not to discontinue the drug are split.
Most providers recommend that men stop using finasteride for at least one month prior to conceiving. Other doctors claim that quitting finasteride is unnecessary, and come at the expense of lost hair. They even go so far as to say there’s “no evidence” that finasteride use for men during windows of conception leads to different health outcomes for their future offspring.
So, which position holds more merit? We’ll detail both sides of the scientific argument below and provide our own take on the data. Then, we’ll reveal a strategy men can employ to temporarily quit finasteride — within a window that shouldn’t compromise any hair gains — and use that window to conceive without (hopefully) losing additional hair.
It all boils down to the length of time it takes for finasteride’s hair growth-promoting effects to wear off versus the length of time the medication takes to clear from the system. Fortunately, there’s a difference here that is in favor of a reproductive window.
Should Men Stop Using Finasteride Before Or During Conception?
In one research article 2001, a group of family physicians examine the perceived versus realized risk of men using oral finasteride during windows of conception.[3]https://www.ncbi.nlm.nih.gov/pmc/articles/PMC2018472/pdf/11785276.pdf
First, the authors review evidence surrounding just how much of a daily 1mg finasteride pill ends up detectable in semen:
“In one study, semen levels were measured in 35 men taking 1 mg of finasteride daily for 6 weeks. Highest level measured was 1.52 ng/mL; mean level was 0.26 ng/mL.”
Then, the authors sought to use these numbers to estimate the total exposure of finasteride to a developing fetus — throughout a pregnancy — due to daily unprotected sex.
“Assuming a 100% vaginal absorption through a 5-mL ejaculate per day, women would be exposed to 7.6 ng/d, a negligible amount.”
Finally, the authors contextualized that risk by comparing that exposure level of finasteride to the amount that was required to cause birth defects in monkey studies.
“This level is 750 times lower than the “no effect” level for developmental abnormalities in rhesus monkeys.”
For these reasons, the authors conclude that finasteride use — at least in men — probably doesn’t need to be stopped during pregnancy.
The authors go on to state that, at least for men, the major risk of using finasteride during conception might instead be the drug’s temporary reductions to semen counts, which may impact the ability to conceive, but not the actual health of the baby (more on this later). Thus, while on finasteride, it may be more difficult to conceive within the first few months of using finasteride (when sperm parameters decline) if a male has borderline-low semen levels prior to starting the medication.
Beyond this, the authors seem far less concerned about about finasteride’s effects on the actual conception, such as potential congenital disabilities or risks to male fetal development. In fact, they assert that there’s no data that, during conception, the use of finasteride (for males) interferes with reproductive or fetal outcomes. They recommend that men taking oral finasteride keep taking the drug throughout conception.
Unfortunately, this review was conducted in 2001 — when epigenetics was still an emerging field, and when research groups weren’t necessarily aware of other markers worth measuring that might affect the health of fetal development. Today, in order to completely quell concerns of conception windows and finasteride use in men, what we really need to know is:
- Does finasteride use affect sperm parameters in men?
- Is finasteride use associated with epigenetic and/or DNA damage in sperm, and at doses prescribed for androgenic alopecia?
- Are there actual prospective, long-term studies measuring the outcomes of children whose fathers were using finasteride when they were conceived?
In exploring the answers to these questions, we’ll realize the whole debate over finasteride’s use in men during conception is not as clearcut as it may seem.
Finasteride Use In Men While Conceiving: Affect On Children (Unstudied!)
First, it is true that there are no prospective clinical studies tracking birth outcomes across men using vs. not using finasteride compared to (1) their success with conception, and (2) the health of their offspring. So, does that mean we should assume using finasteride as a male — during conception — is safe?
No. It simply means the question hasn’t been studied. Given that the life and health of a newborn is at stake, our position is that it’s probably better to exercise caution than it is to presume the absence of evidence is a signal suggesting that a behavior that has not been adequately studied must be safe.
Secondly, there’s newer data (from later than 2001) suggesting that finasteride may do more than temporarily lower the ability for men to reproduce via reduced sperm counts, and that these changes may come with a heightened risk of reproductive health.
Finasteride Use In Men: Affect On Sperm Parameters (Studied)
The effects of finasteride use on sperm parameters has been studied in humans at doses of 1-5mg. Here’s what the evidence says.
Overstreet et al (1999)
A 1999 study tested the effects of 1mg finasteride daily on sperm parameters in men. After one year, those using finasteride had an 11% decline in ejaculate volume, compared to 8% in the placebo group. The researchers also noted no significant changes to “sperm concentration, total sperm per ejaculate, sperm motility or morphology.” Resultantly, the team concluded that 1mg daily finasteride use “does not affect spermatogenesis of semen parameters” in men.[4]https://pubmed.ncbi.nlm.nih.gov/10492183/
Given that the study was randomized, double-blinded, placebo-controlled, used the standard dose of finasteride for androgenic alopecia, and ran a full year — many people use this study as justification that finasteride use (in men) probably does not have deleterious effects on reproduction.
Unfortunately, there are two problems with this reasoning.
The first problem is that the study doesn’t actually measure reproductive outcomes, nor does it measure epigenetic changes to sperm. Rather, the study only measure changes to sperms’ histological features: its concentration, sperm per ejaculate, sperm motility, sperm morphology, and semen volume. From a safety perspective, the clinical results are a positive signal. But without long-term studies on fetal outcomes for men using finasteride during conception, they don’t actually answer the question of whether finasteride use in men affect the way their offspring develop.
The second problem is that there are other studies on finasteride that add nuance to finasteride’s safety on sperm parameters — particularly at 5mg doses.
Amory et al (2007)
A 2007 study tested the effects of daily use of 5mg finasteride or 0.5mg dutasteride on semen parameters in healthy men versus placebo. Over six months, the authors found that daily doses of 5mg of finasteride or 0.5mg of dutasteride significantly reduced sperm counts, and by 25-35%. However, at the 12-month mark of continued use, sperm counts for finasteride were still below baseline (i.e., -14.5%), but no longer statistically significantly lower than when the study began.[5]https://academic.oup.com/jcem/article/92/5/1659/2598215
For these reasons, some researchers claim that the effects of finasteride on sperm parameters — if any — are temporary and resolve with continued use at 5mg daily doses, if those changes even exist at all at lower doses (i.e., 1mg).
This should be the end of the story, right? After all, most men are prescribed finasteride at 1mg daily for androgenic alopecia. So, if at 1mg daily there appears to be no effect on sperm parameters, and at 5mg daily the effect seems to diminish with continued use, then men must be in-the-clear to use finasteride while conceiving. Correct?
No.
Again, there are no randomized controlled clinical trials measuring long-term outcomes of children whose fathers were using finasteride before/during their conception. Moreover, sperm counts, motility, and morphogenesis are all histological features of sperm. What isn’t measured in these study is the effect of DNA expression on sperm (i.e., epigenetics). Keep in mind that you can have plenty of sperm that looks healthy, swims effectively, appears normal… but still carries with it genetic expressions that insinuate damage or a heightened potential of birth defects for the fetus.
So, is there any data giving us insights into the potential for finasteride to cause epigenetic changes to sperm (or damage to sperm) that might otherwise affect reproductive capacity and/or fetal outcomes? And no, we’re not talking mouse models that administer high-dose finasteride (which aren’t always applicable to human research, despite what hair loss forums may tell you).[6]https://www.mdpi.com/1467-3045/43/2/62 We’re talking about human evidence.
Yes, there is evidence. And while that evidence isn’t high-quality, it’s still worth discussing.
Finasteride And Infertility In Men: Tu HY, Zini A. (2011), Şalvarci A, Istanbulluoğlu O. (2012)
In 2011 and 2012, two separate case reports were published — each on a male using finasteride long-term who was having trouble conceiving with his respective partner.
Researchers examined sperm morphology — as the studies above did — which appeared normal. But then they examined the sperm through another endpoint: a sperm DNA fragmentation index. This is a measurement to approximate DNA damage (i.e., fragmentation). In both cases, sperm DNA fragmentation was elevated. After discontinuing finasteride, one case report saw sperm DNA fragmentation reduced from 30% to 16.5% within six months.[7]https://pubmed.ncbi.nlm.nih.gov/21292254/ The other case report noted similar improvements to DNA fragmentation, and the successful conception of a baby after discontinuing the drug.[8]https://pubmed.ncbi.nlm.nih.gov/23070721/ The implication: that finasteride use in some men may damage the DNA of sperm, and that discontinuing the drug can improve these outcomes.
Please note: these are case reports, and with such uncontrolled (and unrobust data), there is always the possibility that something aside from the discontinuance of finasteride might be explaining these results. For instance, upon receiving this news, both men featured in the case reports might not have only stopped finasteride, but also addressed other aspects of health to reduce their risk of sperm DNA fragmentation. Examples include supplementing with vitamin D, incorporating more daily activity into their lives, quitting alcohol, getting more consistent sleep, etc.
As such, there’s always the possibility that finasteride was not the majority causative agent in either outcomes.
Our Perspectives: Should Men Continue Using Finasteride While Trying To Have a Baby?
Given the balance of evidence, we feel that men using finasteride should perhaps exercise caution about continuing the drug while also trying to grow their families.
Unfortunately, this position puts many men in an uncomfortable situation. They might feel as though they need to withdraw from a hair-saving drug in order to minimize risks that aren’t necessarily clear, based on the clinical data. Again, those long-term studies on children whose fathers conceived them while using finasteride haven’t yet occurred. They may never occur.
At the same time, this “abundance of caution” comes at a tall expense: lost hair. After all, clinical studies show that after quitting finasteride, any hair that was preserved by the drug is lost and, soon after, hair loss continues at its normal rate.
These risks-benefits are not ours to make for anyone. We’re just here to communicate the data, and the debate. Risk tolerances vary depending on the person, and for many couples, the continued use of finasteride might be the decision made by the male during the windows of conception. This is a decision that shouldn’t be made by us; it should be made by you along with the counseling of your doctor(s).
Nonetheless, if you are looking for an approach to minimize the risks to a developing fetus while simultaneously preserving hair, there is a happy middle ground… and perhaps a way to get the best of both worlds.
Consider Quitting Finasteride Temporarily During Conception
Finasteride is a drug that has a terminal half-life of 5-7 hours, and a biological half-life of around two weeks. In other words, while it takes 5-7 hours for half of the finasteride in your bloodstream to metabolize, it takes 2+ weeks for half of the effects from finasteride use — i.e., the lowering of dihydrotestosterone — to go away. For these reasons, it is estimated that after quitting finasteride, it still takes ~30 days for finasteride (and its effects) to completely leave the body.
This is why most physicians recommend beginning trying to conceive after 30+ days away from finasteride (if female). But after quitting finasteride, how long does it take before hair loss starts to pick back up again?
According to the clinical literature, longer than four weeks. In fact, one study showed that, after one full year of use, men who quit finasteride were still above their baseline hair counts a year after leaving the medication.[9]https://www.sciencedirect.com/science/article/pii/S0022202X15529357 Another study showed that after one year of finasteride use, men who switched to every-other-month of daily medication had the same hair growth outcomes as men who still used the drug every day of the year.[10]https://pubmed.ncbi.nlm.nih.gov/15319158/
Taken together, these studies imply that finasteride’s terminal and biological half-lives might enable a key window whereby men can transition off the drug, conceive without detectable levels of finasteride in their sperm (and/or any adverse effects on sperm from finasteride use), then hop back on the drug — all with little (if any) risk to their hair.
Based on the current data, this window appears to be 1-3 months after quitting finasteride. Within that time, hair loss from withdrawal of the drug should be relatively minimal. And with a two-month reproductive window, this should hopefully be enough time to give couples a good chance to conceive.
What About Topical Finasteride?
For women, the use of topical finasteride within a month before conceiving, during pregnancy, or while breastfeeding is not recommended. This is because a portion of the drug will still go systemic, thereby potentiating adverse events to the developing baby.
For men, there is not yet any data to answer this question — but out of caution, many physicians will just say, “Don’t do it” However, it’s likely that the risks with topical finasteride — especially at lower exposure volumes (0.1 mg daily) — are much smaller than any risks with the oral formulations of the drug (due to less systemic exposure and thereby lower concentrations in the semen).
That said, for those using topical finasteride while starting a family, the Perfect Hair Health team recommends doing everything possible to minimize topical finasteride exposure to a partner while they are pregnant. We’ll have articles on how to do this in the near-future.
References[+]
References ↑1 https://rep.bioscientifica.com/configurable/content/journals$002frep$002f155$002f3$002fREP-17-0380.xml ↑2 https://dailymed.nlm.nih.gov/dailymed/lookup.cfm?setid=f96c6acd-4d02-4ece-bd54-2d5a35aab7f5#section-12.2 ↑3 https://www.ncbi.nlm.nih.gov/pmc/articles/PMC2018472/pdf/11785276.pdf ↑4 https://pubmed.ncbi.nlm.nih.gov/10492183/ ↑5 https://academic.oup.com/jcem/article/92/5/1659/2598215 ↑6 https://www.mdpi.com/1467-3045/43/2/62 ↑7 https://pubmed.ncbi.nlm.nih.gov/21292254/ ↑8 https://pubmed.ncbi.nlm.nih.gov/23070721/ ↑9 https://www.sciencedirect.com/science/article/pii/S0022202X15529357 ↑10 https://pubmed.ncbi.nlm.nih.gov/15319158/ Want help with your hair regrowth journey?
Get personalized support, product recommendations, video calls, and more from our researchers, trichologists, and PhD's dedicated to getting you the best possible outcomes.
Learn More
Perfect Hair Health Team
"... Can’t thank @Rob (PHH) and @sanderson17 enough for allowing me to understand a bit what was going on with me and why all these [things were] happening ... "

 — RDB, 35, New York, U.S.A.
— RDB, 35, New York, U.S.A."... There is a lot improvement that I am seeing and my scalp feel alive nowadays... Thanks everyone. "

 — Aayush, 20’s, Boston, MA
— Aayush, 20’s, Boston, MA"... I can say that my hair volume/thickness is about 30% more than it was when I first started."

 — Douglas, 50’s, Montréal, Canada
— Douglas, 50’s, Montréal, CanadaWant help with your hair regrowth journey?
Get personalized support, product recommendations, video calls, and more from our researchers, trichologists, and PhD's dedicated to getting you the best possible outcomes.
Join Now - Mission Statement