- About
- Mission Statement
Education. Evidence. Regrowth.
- Education.
Prioritize knowledge. Make better choices.
- Evidence.
Sort good studies from the bad.
- Regrowth.
Get bigger hair gains.
Team MembersPhD's, resarchers, & consumer advocates.
- Rob English
Founder, researcher, & consumer advocate
- Research Team
Our team of PhD’s, researchers, & more
Editorial PolicyDiscover how we conduct our research.
ContactHave questions? Contact us.
Before-Afters- Transformation Photos
Our library of before-after photos.
- — Jenna, 31, U.S.A.
I have attached my before and afters of my progress since joining this group...
- — Tom, 30, U.K.
I’m convinced I’ve recovered to probably the hairline I had 3 years ago. Super stoked…
- — Rabih, 30’s, U.S.A.
My friends actually told me, “Your hairline improved. Your hair looks thicker...
- — RDB, 35, New York, U.S.A.
I also feel my hair has a different texture to it now…
- — Aayush, 20’s, Boston, MA
Firstly thank you for your work in this field. I am immensely grateful that...
- — Ben M., U.S.A
I just wanted to thank you for all your research, for introducing me to this method...
- — Raul, 50, Spain
To be honest I am having fun with all this and I still don’t know how much...
- — Lisa, 52, U.S.
I see a massive amount of regrowth that is all less than about 8 cm long...
Client Testimonials150+ member experiences.
 Scroll DownPopular Treatments
Scroll DownPopular Treatments- Treatments
Popular treatments. But do they work?
- Finasteride
- Oral
- Topical
- Dutasteride
- Oral
- Topical
- Mesotherapy
- Minoxidil
- Oral
- Topical
- Ketoconazole
- Shampoo
- Topical
- Low-Level Laser Therapy
- Therapy
- Microneedling
- Therapy
- Platelet-Rich Plasma Therapy (PRP)
- Therapy
- Scalp Massages
- Therapy
More
IngredientsTop-selling ingredients, quantified.
- Saw Palmetto
- Redensyl
- Melatonin
- Caffeine
- Biotin
- Rosemary Oil
- Lilac Stem Cells
- Hydrolyzed Wheat Protein
- Sodium Lauryl Sulfate
More
ProductsThe truth about hair loss "best sellers".
- Minoxidil Tablets
Xyon Health
- Finasteride
Strut Health
- Hair Growth Supplements
Happy Head
- REVITA Tablets for Hair Growth Support
DS Laboratories
- FoliGROWTH Ultimate Hair Neutraceutical
Advanced Trichology
- Enhance Hair Density Serum
Fully Vital
- Topical Finasteride and Minoxidil
Xyon Health
- HairOmega Foaming Hair Growth Serum
DrFormulas
- Bio-Cleansing Shampoo
Revivogen MD
more
Key MetricsStandardized rubrics to evaluate all treatments.
- Evidence Quality
Is this treatment well studied?
- Regrowth Potential
How much regrowth can you expect?
- Long-Term Viability
Is this treatment safe & sustainable?
Free Research- Free Resources
Apps, tools, guides, freebies, & more.
- Topical Finasteride Calculator
- Interactive Guide: What Causes Hair Loss?
- Free Guide: Standardized Scalp Massages
- 7-Day Hair Loss Email Course
- Ingredients Database
- Interactive Guide: Hair Loss Disorders
- Treatment Guides
- Product Lab Tests: Purity & Potency
- Evidence Quality Masterclass
More
Articles100+ free articles.
-
Cannabidiol (CBD) Increases Hair Counts By 246%? Not So Fast.
-
Creatine: Does It Worsen Hair Loss? It Depends On The Hair Loss Type.
-
Can Progesterone Improve Hair Regrowth?
-
CRABP2: Can This Gene Predict Regrowth From Retinoids?
-
BTD: Can This Gene Predict Regrowth From Biotin?
-
COL1A1: Can This Gene Predict Regrowth From Collagen Support?
-
2dDR For Hair Loss: What Do We Know So Far About This Sugar?
-
CYP19A1: Can This Gene Predict Regrowth From Hormone Therapy?
PublicationsOur team’s peer-reviewed studies.
- Microneedling and Its Use in Hair Loss Disorders: A Systematic Review
- Use of Botulinum Toxin for Androgenic Alopecia: A Systematic Review
- Conflicting Reports Regarding the Histopathological Features of Androgenic Alopecia
- Self-Assessments of Standardized Scalp Massages for Androgenic Alopecia: Survey Results
- A Hypothetical Pathogenesis Model For Androgenic Alopecia:Clarifying The Dihydrotestosterone Paradox And Rate-Limiting Recovery Factors
Menu- AboutAbout
- Mission Statement
Education. Evidence. Regrowth.
- Team Members
PhD's, resarchers, & consumer advocates.
- Editorial Policy
Discover how we conduct our research.
- Contact
Have questions? Contact us.
- Before-Afters
ArticlesMicroneedling the Scalp: Does it Cause Scarring?
First Published May 31 2024Last Updated Oct 29 2024Natural Remedies Researched & Written By:Sarah King, PhD
Researched & Written By:Sarah King, PhD Reviewed By:Rob English, Medical Editor
Reviewed By:Rob English, Medical Editor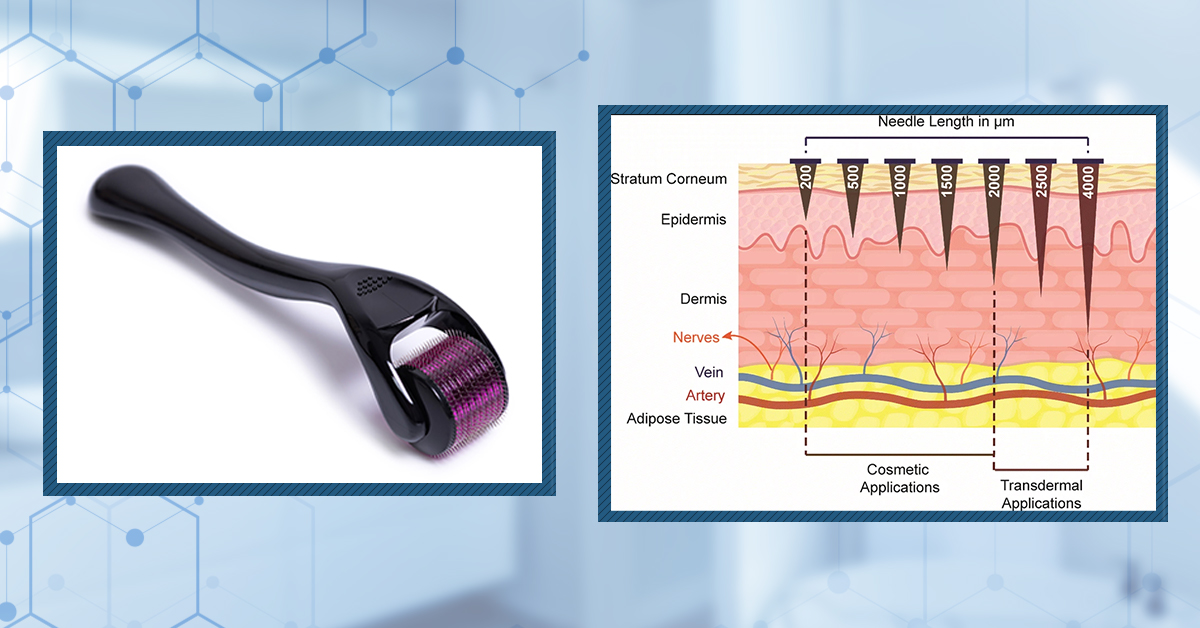
Want help with your hair regrowth journey?
Get personalized support, product recommendations, video calls, and more from our researchers, trichologists, and PhD's dedicated to getting you the best possible outcomes.
Learn MoreArticle Summary
Can repeated microneedling on the scalp cause scarring? There aren’t yet long-term studies answering this question. On the one hand, microneedling increases neocollagenesis (i.e., the formation of new collagen, or skin tissue). On the other hand, studies show that microneedling-induced collagen is well-organized and different from the imperfect collagen seen in scars. Three-month case studies show no fibrosis after microneedling the scalp. Long-term studies on facial skin show a reduction to fibrosis with repeated microneedling. Finally, 20+ year outcomes from patients who received autologous split-thickness grafts harvested from the scalp suggest that a much more aggressive wound-scraping procedure also carries a low risk of scalp scarring – mainly due to the dense population of stem cells in the scalp. In this article, we review the latest data and assess scarring risks across microneedling depths, frequencies, and session timings.
Full Article
In the last decade, interest in microneedling has exploded, particularly among those using these devices as an adjuvant treatment for androgenic alopecia. As of today, dozens of clinical studies suggest that microneedling can improve hair counts through a range of mechanisms – all through the repeated generation of micro-wounds on the scalp.
But as with any wounding-based therapy, there are concerns of scarring. Wounds – when incurred deeply enough (or frequently enough) – carry a risk of imperfect healing, which wold result in disorganized collagen buildup colloquially referred to as fibrosis (scar tissue).
So, does microneedling the scalp carry a risk of scarring? Does the risk change over 1, 2, or even 5+ year periods?
Of course, the answer depends on the needle penetration depth, the devices used, the frequency of treatments, and an individual’s skin type and healing capacity. In this article, we’ll assess a range of clinical studies to help us answer if microneedling the scalp might lead to scar tissue long-term, and if so, what we can do to mitigate those risks.
What are the Benefits of Microneedling?
There are (at least) two ways that microneedling is suspected to improve hair growth outcomes:
1. Microneedling triggers the release of growth factors and proteins linked to new hair growth.
When the needles penetrate the skin, they cause acute inflammation, which prompts the body to send hormones, growth factors, and signaling proteins to the damaged areas for wound repair. Over multiple sessions and months, these factors help produce new collagen, form new blood vessels, and reduce scarring.[1]Singh, A., Yadav, S. (2016). Microneedling: Advances and widening horizons. Indian Dermatology Online Journal. 7(4). 244-254. Available at: https://doi.org/10.4103-5178.185468 Additionally, these growth factors and proteins are closely tied to the anagen (growth) phase of the hair cycle.[2]Kim, Y. S., Jeong, K.H., Kim, J.E., Woo, Y.J., Kim, B.J., Kang, H. (2016). Repeated microneedle stimulation induces enhanced hair growth in a murine model. Annals of Dermatology. 28(5). 586-592. … Continue reading

Figure 1: The effect of microneedling on different factors involved in hair follicle growth. The 0.5 mm microneedle group significantly increased all factors involved in hair follicle growth compared to the control. The 0.25 mm microneedle group significantly increased levels of Wnt3a and Wnt10b mRNA.[3]Kim, Y. S., Jeong, K.H., Kim, J.E., Woo, Y.J., Kim, B.J., Kang, H. (2016). Repeated microneedle stimulation induces enhanced hair growth in a murine model. Annals of Dermatology. 28(5). 586-592. … Continue reading
2. Microneedling boosts the absorption of topical treatments, like minoxidil.
Besides its other effects, microneedling creates temporary micro-tears in the outer layers of the scalp skin. These layers usually serve as a barrier, making it harder for topicals to penetrate the dermis and reach the hair follicle base. By creating micro-wound channels, microneedling improves the absorption of topical treatments, potentially enhancing their effects.[4]Fertig, R.M., Gamret, A.C., Cervantes, J., Tosti, A. (2017). Microneedling for the treatment of hair loss? Journal of the European Academy of Dermatology and Venereology. 32(4). 564-569. Available … Continue reading Furthermore, the wounds increase the activity of the enzyme sulfotransferase, which is necessary to convert topical minoxidil from its inactive to its active form, allowing it to attach to hair follicle cells and be effective.[5]Sharma, A., Surve, R., Dhurat, R., Sinclair, R., Tan, T., Zou, Y., Muller Ramos, P., Wambier, C., Verner, I., Kovacevic, M., Goren, A. (2020). Microneedling improves minoxidil response in … Continue reading Thus, clinical studies show that microneedling can significantly boost the effectiveness of minoxidil, potentially by up to 400% compared to using minoxidil alone.
According to current research, it is generally agreed that microneedling devices with a 1.5-mm needle length and 192-count needles are effective when used at 1-3 weeks intervals. We cover studies looking at needle depth and frequency here.
So, we know the potential benefits of microneedling, but what effect could it have on the scalp long-term?
Microneedling Lays Down New Collagen. Is This Collagen “Scarring?”
Microneedling induces the formation of new collagen, a process known as neocollagenesis, which can continue for months after your last microneedling session. Histological examination of skin treated with 4 microneedling sessions 1 month apart shows up to a 400% increase in collagen and elastin deposition up to 6 months after treatment, with normal histological structures observed up to 1-year post-op.[6]Singh, A., Yadav, S. (2016). Microneedling: Advances and Widening Horizons. Indian Dermatology Online Journal. 7(4). 244-254. Available at https://doi.org/10.4103/2229-5178.185468 This indicates that microneedling leads to an increase in organized collagen deposition.
While some might worry that collagen production could lead to scarring, it’s crucial to differentiate between the types of collagen formed.
Neocollagenesis, the process by which new collagen is laid down after microneedling, results in organized, structured collagen networks. This is in contrast to the disorganized collagen bundles found in scar tissue, which form in a haphazard, irregular pattern.
A study was conducted on 24 participants with post-acne atrophic scarring who were treated with either a derma roller + trichloroacetic acid (TCA 15%), Derma roller + PRP, or derma roller alone for a total of 6 bi-weekly treatments.[7]El-Domyati, M., Abdel-Wahab, H., Hossam, A. Microneedling combined with platelet-rich plasma or trichloroacetic acid peeling for management of acne scarring: A split-face clinical and histologic … Continue reading Upon histochemical evaluation, it was found that all three groups (including the derma roller alone) led to more dense collagen bundles that were more organized and more parallel to the epidermis after 3 months of treatment (Figure 2).

Figure 2. Histochemical staining of facial skin before treatment and after 3 months of treatment. The collagen bundles are more densely packed and organized after three months of treatment.[8]El-Domyati, M., Abdel-Wahab, H., Hossam, A. (2017). Microneedling combined with platelet-rich plasma or trichloroacetic acid peeling for management of acne scarring: A split-face clinical and … Continue reading
Thus, according to this histological study on facial skin, scarring appears to improve from repeated microneedling.
Factors Influencing Collagen Structure
- Cross-Hatching Patterns: Healthy collagen produced through microneedling tends to have organized cross-hatchings, enhancing skin texture and strength. Scar tissue collagen, on the other hand, is characterized by disorganized cross-hatchings.
- Replacement Context: Neocollagenesis replaces subcutaneous fat or previously scarred skin, contributing to a more refined skin appearance.[9]Tuchayi, S.M., Khachatryan, Y., Anderson, R.R., Wang, J.S., Wein, M.N., Garibyan, L. (2023). Selective reduction of visceral adipose tissue with injectable ice slurry. Scientific Reports. 12(16350). … Continue reading Scar tissue often replaces healthy tissue, leading to raised, discolored, or textured skin. Functionally, scar tissue may also lack the elasticity and strength of normal skin, restricting movement or sensation.
- Quantity of Collagen: The amount of collagen produced also plays a role. Controlled collagen production through microneedling results in a balanced and beneficial tissue structure, whereas excessive collagen can lead to hypertrophic scars or keloids.
Could Microneedling Cause Scarring Long-Term?
Since microneedling creates in tiny punctures in the skin’s epidermal and dermal layers, which generate an inflammatory response, it’s understandable to worry that repeated treatments might result in scarring. This is a concern for hair regrowth, as hair cannot grow as effectively in scar tissue.
So, might long-term microneedling undermine the use of this therapy for better hair growth? Again, long-term data are limited. So to best approximate an answer, we’ll need to expand our scope and look at related studies across three wounding domains:
- Microneedling the scalp (short-term studies exist)
- Microneedling the face (medium-term studies exist)
- Autologous split-thickness grafts harvested from the scalp (a much more extreme procedure than microneedling, whereby 20+ year studies exist).
A Systematic Review Of Microneedling: Effects On Facial Scars
One systematic review examined the use of microneedling for the treatment of atrophic scars – typically caused by facial acne. It suggested that microneedling is actually an effective treatment for improving the appearance of atrophic scarring.[10]Sitohand, I.B.S., Sirait, S.A.P., Suryanegara, J. (2021). Microneedling in the treatment of atrophic scars: a systematic review of randomised controlled trials. International Wound Journal. 18(5). … Continue reading
- Of the nine studies in the systematic review, no serious adverse events were observed, the most common being transient redness, swelling, and pinpoint bleeding.
- Each study found that microneedling reduces acne scarring, with more improvement when combined with topical treatments like polylactic acid, trichloroacetic acid (TCA), and Jessner’s solution (a light to medium chemical peel containing salicylic acid, lactic acid, and resorcinol).
- Moreover, some of the studies lasted up to five months, indicating that medium-term use can still be safe.
A larger, long-term study was conducted for 120 patients with facial and nonfacial scarring from acne, trauma, and surgery.[11]Alster, T.S., Li, M.K.Y. (2019). Microneedling of Scars: A Large Prospective Study with Long-Term Follow-Up. Plastic and Reconstructive Surgery. 145(2). 358-364. Available at: … Continue reading Follow-ups were conducted 1, 3, 6, and 12 months after treatment. Patients received one to six consecutive monthly microneedling treatments.
The researchers observed at least a 50% improvement in all scarring after an average of 2.5 treatments. 80% of patients had 50 – 75% improvement, and 65% of patients showed 75% or more improvement. Below, you can see the effect of microneedling on a surgical scar six months after treatment, which suggests continuous collagen remodeling and sustained improvements to skin quality even after treatment has finished (Figure 3).

Figure 3. Surgical scar on the nose before (left) and 6 months after (right) two microneedling treatments.[12]Alster, T.S., Li, M.K.Y. (2019). Microneedling of Scars: A Large Prospective Study with Long-Term Follow-Up. Plastic and Reconstructive Surgery. 145(2). 358-364. Available at: … Continue reading
Are There Any Studies Exploring Scalp Microneedling & Scarring?
Yes, but they are incredibly limited. Here’s what we know so far.
3-Month Case Study On Scalp Microneedling: Effects On Scalp Scarring
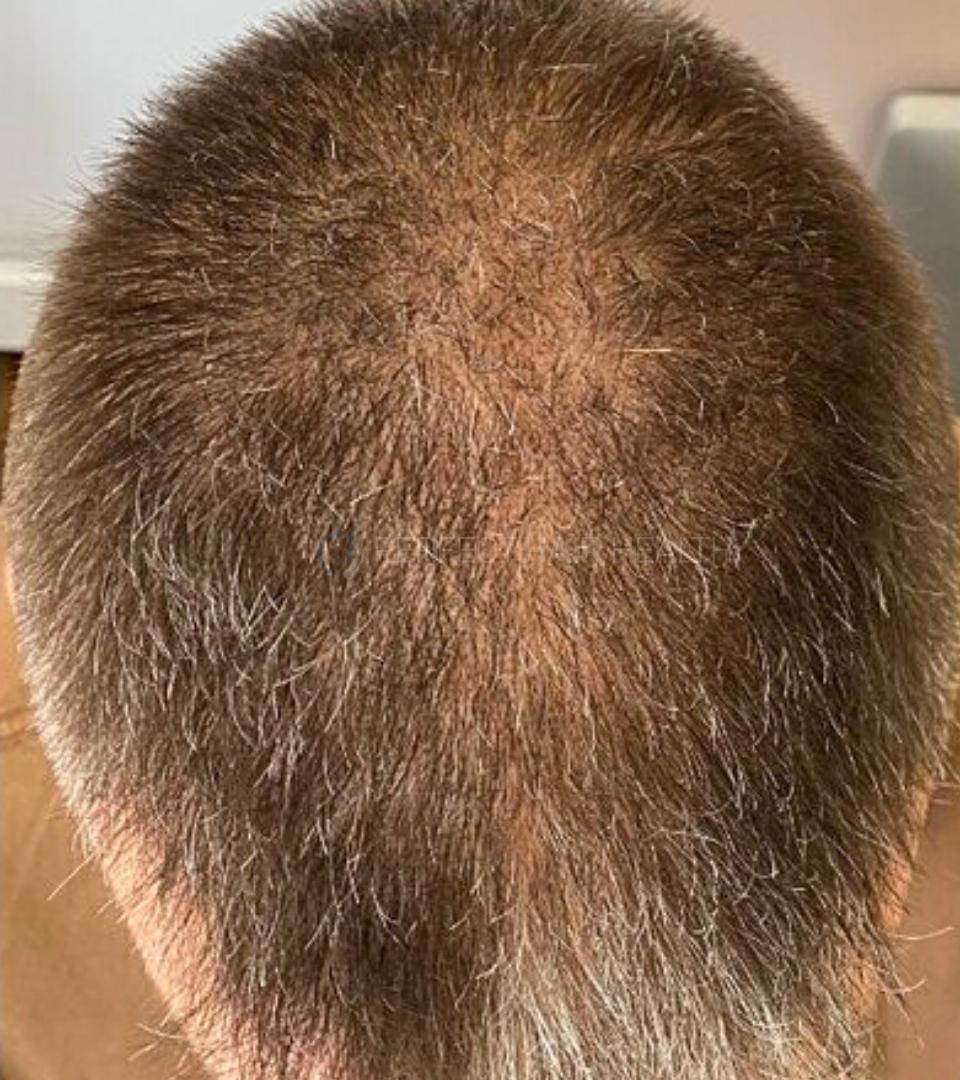
This paper presented a case study of a 37-year-old woman with a 15-year history of female pattern hair loss. For three sessions, the patient underwent microneedling with a 2 mm roller device at monthly intervals. Two 4 mm punch biopsies were collected before treatment, and one was collected after treatment (close to the area of the first punch biopsy site). The post-treatment biopsy showed no scarring effect on the scalp (Figure 4).[13]Basillo, F.M.A.B., Brenner, F.M., Werner, B. (2021). Microneedling for female pattern hair loss: case report and histopathological changes. Surgical and Cosmetic Dermatology. 14. E20220074. Available … Continue reading

Figure 4: Pattern of hair thinning on a female patient’s scalp (A) before microneedling and (B) after microneedling. No visible scarring was observed.[14]Basillo, F.M.A.B., Brenner, F.M., Werner, B. (2021). Microneedling for female pattern hair loss: case report and histopathological changes. Surgical and Cosmetic Dermatology. 14. E20220074. Available … Continue reading
32-Week Study: Microneedling at 1.5mm, Once Every 4 Weeks
Another study investigated the safety (and efficacy) of microneedling in men with AGA. 30 male participants with androgenic alopecia were included in the study and randomly allocated into two groups (roller and tattoo cartridge).[15]Kakizaki, P., Contin, L.A., Barletta, M., Machado, C.J., Michalany, N.S., Valente, N.Y.S., Donati, A. (2023). Efficacy and safety of scalp microneedling in male pattern hair loss. Skin Appendage … Continue reading Microneedling sessions were done once every four weeks for a total of four times, and both devices were set to a 1.5 mm depth. Follow-up visits were conducted four and sixteen weeks after the last treatment. The total study time was 32 weeks.
At the end of the study, investigators observed new collagen bundles and the destruction of elastic fibers in some of the mirconeedling patients.
At a glance, this might read like bad news, and perhaps an indication that scalp microneedling might lead to scarring. However, here’s the problem with jumping to that conclusion:
- Increased collagen bundles are hallmarks of scarring… depending on how those collagen bundles are organized. If they’re well-organized – which is what prior microneedling studies on the scalp & skin indicate – then these new collagen bundles probably aren’t a problem.
- The role of elastin (and what it creates: elastic fibers) in scarring is not fully understood. Studies show that both a loss of elastic fibers and an increase in elastic fibers can both result in scarring, which complicated the interpretation of their presence in this study.[16]Roten SV, Bhat S, Bhawan J. Elastic fibers in scar tissue. J Cutan Pathol. 1996 Feb;23(1):37-42. doi: 10.1111/j.1600-0560.1996.tb00775.x. PMID: 8720985.
- Increased collagen deposition and elastin are well-documented hallmarks of the balding process. They’re found in the scalps of people with androgenic alopecia, regardless of whether they’re microneedling or not. For reference, excessive collagen deposition is found in 40% of scalps affected by androgenic alopecia, and elastin fibers are speculated by some to be a driving force (and rate-limiting recovery factor) of the balding process.[17]Asfour, L., Cranwell, W., Sinclair, R. (2023). Male Androgenetic Alopecia. Available from: https://www.ncbi.nlm.nih.gov/books/NBK278957/ (Accessed: 17 May 2024)[18]Rushton DH, Westgate GE, Van Neste DJ. Following historical “tracks” of hair follicle miniaturisation in patterned hair loss: Are elastin bodies the forgotten aetiology? Exp Dermatol. … Continue reading
- Therefore, the presence of collagen bundles and elastolysis (i.e., elastin surrounding elastic fibers) noted in some patients in this study doesn’t really tell us anything. Were these observations caused by microneedling? Or were they caused by the natural advancement of the balding process? Were the collagen bundles well-organized, or were they disorganized? Was the elastolysis an indication of scarring to come, protection from scarring, or just the natural advancement of balding? The study wasn’t designed to answer these questions, so we’re left with lots of noise and very little room to interpret the meaning of these findings.
So, what if we extend our scope beyond microneedling and explore more aggressive forms of scalp wounding? Might this establish an upper limit for how much wounding our scalps can experience before triggering a scarring response? We can (partly) explore this with something called split-thickness autologous grafts taken from the scalp skin.
Split-Thickness Autologous Grafts, Harvested From The Scalp: Long-Term Outcomes
Studies have shown that the scalp can withstand a great deal of trauma and still recover its hair growth. In cases of childhood burns, split skin grafts are taken from the scalp. A split skin (or split-thickness graft) is a thin layer of skin shaved from the target area, usually using a dermatome which is then grafted onto the injured area to assist with wound healing.[19]Braza, M.R., Fahrenkopf, M.P. (2023). Split-thickness skin grafts. StatPearls. Available at: https://www.ncbi.nlm.nih.gov/books/NBK551561/ (Accessed: 23 May 2024)
Some advantages of using scalp skin include less pain, large surface area and richness of stem cells in the hair follicle bulge (where the stem cells reside) that promotes faster wound healing as long as it is preserved during skin harvest. As the bulge typically resides 1-1.8 mm into the scalp, hypothetically, the skin and hair can more rapidly and healthfully regenerate, provided the scalp retains the bulge to facilitate cell regeneration. Moreover, multiple harvests can be conducted in the same areas of the scalp due to the scalp’s ability to heal faster. It is also considered cosmetically favorable because as the hair regrows, it conceals the donor site, providing a cosmetically favorable outcome.[20]Roodbergen, D.T., Vloemans, A.F.P.M., Rashaan, Z.M., Broertjes, J.C., Breederveld, R.S. (2016). The scalp as a donor site for skin grafting in burns: retrospective study on complications. Burns … Continue reading
Firstly, the scalp is shaved, disinfected, and infiltrated with a sterile physiological solution to create a cushion that allows for skin harvesting. Dermatoming typically is conducted at a thickness of 0.2-0.3 mm, and then strips of scalp skin are collected for grafting before washing and bandaging (Figure 5)

Figure 5: (A) Preparation of the donor site. The donor site is injected with a physiological solution. (B) Harvesting of the split-thickness skin graft using a dermatome. (C) Donor site after harvesting (not shown). (D) Donor site after dressing (not shown).[21]Roodbergen, D.T., Vloemans, A.F.P.M., Rashaan, Z.M., Broertjes, J.C., Breederveld, R.S. (2016). The scalp as a donor site for skin grafting in burns: retrospective study on complications. Burns & … Continue reading
Based on the published evidence, the risk of scarring or alopecia from the scalp donor site after split-thickness grafting is low.
One case report specifically states that hypertrophic or keloid scarring has never been reported following split-thickness skin grafts from the scalp, even in patients showing keloid formation in other areas.[22]Sun, L., Patel, A.J.K. (2021). Outcomes of split vs full-thickness skin grafts in scalp reconstruction in outpatient local anaesthetic theatre. Scars, burns and healing. 21(7). 1-6. Available at: … Continue reading
Another study evaluated 105 scalp grafts in 93 burn patients over 7 years. The results showed no alopecia or scarring at any of the donor sites and fast healing of the scalp after taking the grafts.[23]Roodbergen, D.T., Vloemans, A.F.P.M., Rashaan, Z.M., Broertjes, J.C., Breederveld, R.S. (2016). The scalp as a donor site for skin grafting in burns: retrospective study on complications. Burns … Continue reading
Another study compared 29 split-thickness skin grafts taken from the thigh and 37 taken from the scalp with a one-year follow-up in children.[24]Martinot, V., Mitchell, V., Fevrier, P., Duhamel, A., Pellerin, P. (1994). Comparative study of split-thickness skin grafts taken from the scalp and thigh in children. Burns. 20(2). 146-150. … Continue reading
The researchers found that while harvesting was more difficult from the scalp, it resulted in no after-effects and no alopecia, whereas after-effects were evident in grafts taken from the thigh. Furthermore, the donor site was not visible for two patients in the thigh grafting group, compared to 33 patients in the scalp grafting group (Figure 6).

Figure 5: 18-month-old child’s scalp 1 month after harvesting of a split-thickness skin graft. Hair regrowth covers the effects of scarring.[25]Martinot, V., Mitchell, V., Fevrier, P., Duhamel, A., Pellerin, P. (1994). Comparative study of split-thickness skin grafts taken from the scalp and thigh in children. Burns. 20(2). 146-150. … Continue reading
Another case study details a split-thickness skin graft taken from the scalp using a freehand scalpel technique with an incision of less than 1 mm deep.[26]Maruyama, S. (2019). Harvesting split-thickness skin from the scalp using a scalpel. PRS Global Open. 7(5). e2206. Available at: https://doi.org/10.1097/GOX.0000000000002206 In this case study, four patients had skin harvested from their scalps of different sizes, with the largest being 7.49 x 7.29 cm (Figure 6). As can be seen below, even using this technique, hair grew back completely, with no visible scarring (Figure 7).

Figure 7: Appearance of donor site, before grafting (A), after grafting (B), and 10 months after grafting (C). No scarring or alopecia was observed.[27]Maruyama, S. (2019). Harvesting split-thickness skin from the scalp using a scalpel. PRS Global Open. 7(5). e2206. Available at: https://doi.org/10.1097/GOX.0000000000002206
On the other hand, one study analyzed the results and complications relating to using the scalp as a donor site in a cohort of 25 patients, 15 of whom were of African descent, 9 mixed race, and one Caucasian.[28]van Niekerk, G., Adams, S., Rode, H. (2018). Scalp as a donor site in children: Is it really the best option? Burns. 44(5). 1259-1268. Available at: https://doi.org/10.1016/j.burns.2018.02.021 All of the patients had split-thickness grafts taken from the scalp at a setting of 0.2 mm. It was found that the patients of African descent had longer healing times (15 days compared to 11.8 and 8.5 days, respectively) and higher incidences of complications such as folliculitis, alopecia, visible scars, hypopigmented scars, and hypertrophic scars (Figure 8).

Figure 8. Number of short and long-term complications of split-thickness scalp grafts by ethnicity.[29]van Niekerk, G., Adams, S., Rode, H. (2018). Scalp as a donor site in children: Is it really the best option? Burns. 44(5). 1259-1268. Available at: https://doi.org/10.1016/j.burns.2018.02.021
The researchers hypothesized that these complications were due to the majority of the participants having hair types VI-VIII (which includes coiled, very coiled, and zig-zag coiled type hair). This type of hair is typically shorter, grows slower, and with lower hair density than those with hair types I-III. Therefore, the typical benefits observed (such as fast hair growth) may not be seen. The researchers concluded that children of African descent should avoid having split-thickness grafts taken from the scalp due to the risk of complications and scarring.
However, as microneedling is typically less traumatic to the scalp than split-thickness scalp grafts, we think it’s unlikely that these types of complications will occur.
What Are Safe Microneedling Depths, Frequencies, & Procedures?
The short-answer: nobody knows. There isn’t (yet) long-term evidence answering what the best practices are for scalp microneedling in terms of both efficacy (i.e., hair growth) and safety (i.e., no scarring).
Having said that, we think a reasonable protocol might look like this:
- Microneedling penetration depth: up to 0.8 mm. (See this article)
- Microneedling frequency: once every 1-2 weeks. (See this article)
- Microneedling procedure: 5-10 minutes; pinpoint bleeding is not necessary.
These recommendations will change as more data are published.
Final Thoughts
While robust data do not yet exist assessing the risk of scalp scarring and microneedling, here’s what we know so far:
- Short-term studies on scalp microneedling don’t appear to show an increased risk of scarring.
- Medium-term studies on facial tissues show a reduction in scarring appearances following repeated microneedling.
- Long-term studies on a more aggressive wounding procedure – split-thickness autologous grafts harvested from the scalp, where up to 0.5 mm of skin is peeled off the head – also show a low risk of scarring and normal hair regrowth following the procedure.
Microneedling any skin – including the scalp – can increase neocollagenesis (i.e., the formation of new collagen). But this collagen appears to be well-organized. It also appears to replace disorganized collagen bundles characteristic of scar tissue.
It goes without saying that those who have contraindications for wounding-based protocols – i.e., poor wound-healing, a predisposition toward keloid scarring, etc. – should avoid microneedling. As always, speak to your doctor before doing anything. With that in mind, we see the current landscape of data as encouraging.
References[+]
References ↑1 Singh, A., Yadav, S. (2016). Microneedling: Advances and widening horizons. Indian Dermatology Online Journal. 7(4). 244-254. Available at: https://doi.org/10.4103-5178.185468 ↑2, ↑3 Kim, Y. S., Jeong, K.H., Kim, J.E., Woo, Y.J., Kim, B.J., Kang, H. (2016). Repeated microneedle stimulation induces enhanced hair growth in a murine model. Annals of Dermatology. 28(5). 586-592. Available at: https://doi.org/10.5021/ad.2016.28.5.586 ↑4 Fertig, R.M., Gamret, A.C., Cervantes, J., Tosti, A. (2017). Microneedling for the treatment of hair loss? Journal of the European Academy of Dermatology and Venereology. 32(4). 564-569. Available at: https://doi.org/10.1111/jdv.14722 ↑5 Sharma, A., Surve, R., Dhurat, R., Sinclair, R., Tan, T., Zou, Y., Muller Ramos, P., Wambier, C., Verner, I., Kovacevic, M., Goren, A. (2020). Microneedling improves minoxidil response in androgenetic alopecia patients by upregulating follicular sulfotransferase enzymes. Journal of Biological Regulators and Homeostatic Agents. 34(2). 659-661. Available at: https://doi.org/10.23812/19-385-L-51 ↑6 Singh, A., Yadav, S. (2016). Microneedling: Advances and Widening Horizons. Indian Dermatology Online Journal. 7(4). 244-254. Available at https://doi.org/10.4103/2229-5178.185468 ↑7 El-Domyati, M., Abdel-Wahab, H., Hossam, A. Microneedling combined with platelet-rich plasma or trichloroacetic acid peeling for management of acne scarring: A split-face clinical and histologic comparison. Journal of Cosmetic Dermatology. 17. 73-83. Available at: https://doi.org/10.1111/jocd.12459 ↑8 El-Domyati, M., Abdel-Wahab, H., Hossam, A. (2017). Microneedling combined with platelet-rich plasma or trichloroacetic acid peeling for management of acne scarring: A split-face clinical and histologic comparison. Journal of Cosmetic Dermatology. 17. 73-83. Available at: https://doi.org/10.1111/jocd.12459 ↑9 Tuchayi, S.M., Khachatryan, Y., Anderson, R.R., Wang, J.S., Wein, M.N., Garibyan, L. (2023). Selective reduction of visceral adipose tissue with injectable ice slurry. Scientific Reports. 12(16350). Available at: https://doi.org/10.1038/s41598-023-43220-9 ↑10 Sitohand, I.B.S., Sirait, S.A.P., Suryanegara, J. (2021). Microneedling in the treatment of atrophic scars: a systematic review of randomised controlled trials. International Wound Journal. 18(5). 577-585. Available at: https://doi.org/10.1111/iwj.13559 ↑11, ↑12 Alster, T.S., Li, M.K.Y. (2019). Microneedling of Scars: A Large Prospective Study with Long-Term Follow-Up. Plastic and Reconstructive Surgery. 145(2). 358-364. Available at: https://doi/10.1097/PRS.0000000000006462 ↑13 Basillo, F.M.A.B., Brenner, F.M., Werner, B. (2021). Microneedling for female pattern hair loss: case report and histopathological changes. Surgical and Cosmetic Dermatology. 14. E20220074. Available at: https://doi.org/10.5935/scd1984-8773.2022140074 ↑14 Basillo, F.M.A.B., Brenner, F.M., Werner, B. (2021). Microneedling for female pattern hair loss: case report and histopathological changes. Surgical and Cosmetic Dermatology. 14. E20220074. Available at: https://doi.org/10.5935/scd1984-8773.2022140074 ↑15 Kakizaki, P., Contin, L.A., Barletta, M., Machado, C.J., Michalany, N.S., Valente, N.Y.S., Donati, A. (2023). Efficacy and safety of scalp microneedling in male pattern hair loss. Skin Appendage Disorders. 9(1). 18-26. Available at: https://doi.org/10.1159/000526215 ↑16 Roten SV, Bhat S, Bhawan J. Elastic fibers in scar tissue. J Cutan Pathol. 1996 Feb;23(1):37-42. doi: 10.1111/j.1600-0560.1996.tb00775.x. PMID: 8720985. ↑17 Asfour, L., Cranwell, W., Sinclair, R. (2023). Male Androgenetic Alopecia. Available from: https://www.ncbi.nlm.nih.gov/books/NBK278957/ (Accessed: 17 May 2024) ↑18 Rushton DH, Westgate GE, Van Neste DJ. Following historical “tracks” of hair follicle miniaturisation in patterned hair loss: Are elastin bodies the forgotten aetiology? Exp Dermatol. 2022 Feb;31(2):102-109. doi: 10.1111/exd.14393. Epub 2021 Jun 11. PMID: 34008225; PMCID: PMC9290669. (Accessed: 17 May 2024) ↑19 Braza, M.R., Fahrenkopf, M.P. (2023). Split-thickness skin grafts. StatPearls. Available at: https://www.ncbi.nlm.nih.gov/books/NBK551561/ (Accessed: 23 May 2024) ↑20 Roodbergen, D.T., Vloemans, A.F.P.M., Rashaan, Z.M., Broertjes, J.C., Breederveld, R.S. (2016). The scalp as a donor site for skin grafting in burns: retrospective study on complications. Burns Trauma. 4(20). 1-6. Available at: https://doi.org/10.1186/s41038-016-0042-z ↑21 Roodbergen, D.T., Vloemans, A.F.P.M., Rashaan, Z.M., Broertjes, J.C., Breederveld, R.S. (2016). The scalp as a donor site for skin grafting in burns: retrospective study on complications. Burns & Trauma. 4(20). 1-6. Available at: https://doi.org/10.1186/s41038-016-0042-z ↑22 Sun, L., Patel, A.J.K. (2021). Outcomes of split vs full-thickness skin grafts in scalp reconstruction in outpatient local anaesthetic theatre. Scars, burns and healing. 21(7). 1-6. Available at: https://doi.org/10.1177/20595131211056542 ↑23 Roodbergen, D.T., Vloemans, A.F.P.M., Rashaan, Z.M., Broertjes, J.C., Breederveld, R.S. (2016). The scalp as a donor site for skin grafting in burns: retrospective study on complications. Burns Trauma. 4(20). 1-6. Available at: https://doi.org/10.1186/s41038-016-0042-z ↑24, ↑25 Martinot, V., Mitchell, V., Fevrier, P., Duhamel, A., Pellerin, P. (1994). Comparative study of split-thickness skin grafts taken from the scalp and thigh in children. Burns. 20(2). 146-150. Available at: https://doi.org/10.1016/S0305-4179(06)80012-4 ↑26, ↑27 Maruyama, S. (2019). Harvesting split-thickness skin from the scalp using a scalpel. PRS Global Open. 7(5). e2206. Available at: https://doi.org/10.1097/GOX.0000000000002206 ↑28 van Niekerk, G., Adams, S., Rode, H. (2018). Scalp as a donor site in children: Is it really the best option? Burns. 44(5). 1259-1268. Available at: https://doi.org/10.1016/j.burns.2018.02.021 ↑29 van Niekerk, G., Adams, S., Rode, H. (2018). Scalp as a donor site in children: Is it really the best option? Burns. 44(5). 1259-1268. Available at: https://doi.org/10.1016/j.burns.2018.02.021 Want help with your hair regrowth journey?
Get personalized support, product recommendations, video calls, and more from our researchers, trichologists, and PhD's dedicated to getting you the best possible outcomes.
Learn More
Sarah King, PhD
Dr. Sarah King is a researcher & writer who holds a BSc in Medical Biology, an MSc in Forensic Biology, and a Ph.D. in Molecular and Cellular Biology. While at university, Dr. King’s research focused on cellular aging and senescence through NAD-dependent signaling – along with research into prostaglandins and their role in hair loss. She is a co-author on several upcoming manuscripts with the Perfect Hair Health team.
"... Can’t thank @Rob (PHH) and @sanderson17 enough for allowing me to understand a bit what was going on with me and why all these [things were] happening ... "

 — RDB, 35, New York, U.S.A.
— RDB, 35, New York, U.S.A."... There is a lot improvement that I am seeing and my scalp feel alive nowadays... Thanks everyone. "

 — Aayush, 20’s, Boston, MA
— Aayush, 20’s, Boston, MA"... I can say that my hair volume/thickness is about 30% more than it was when I first started."

 — Douglas, 50’s, Montréal, Canada
— Douglas, 50’s, Montréal, CanadaWant help with your hair regrowth journey?
Get personalized support, product recommendations, video calls, and more from our researchers, trichologists, and PhD's dedicated to getting you the best possible outcomes.
Join Now - Mission Statement